Whiplash Injuries Explained: Whiplash Associated Disorders
- Approximately 15 to 40% of those injured in automobile accidents will struggle with chronic pain for the rest of their life. Journal of the American Academy of Orthopedic Surgeons, 2007
- Whiplash injuries not only increase your chances of chronic neck and shoulder pain, they also increase the probability of other seemingly unrelated health problems. Journal of Clinical Epidemiology, 2001
- Chronic Pain does bad things to people. According to standardized assessment tests, 100% of those struggling with chronic pain caused by whiplash injuries have abnormal psychological profiles. The only way to resolve these abnormal psychological profiles is to relieve / remove the chronic back pain, neck pain and headaches. Counseling / Psychiatry has not been shown to improve the pain nor the psychological profiles of people suffering from the effects of their automobile accident. Pain, 1997
- The longest-running study ever done on whiplash patients looked at the overall health of whiplash patients almost twenty years after their automobile accident. Nearly two decades after their accident, 55% of those patients still deal with chronic pain. Accident Analysis and Prevention, 2002
- Unless you have a fracture or specific ligament tear, Cervical Collars are no longer recommended for treating patients with whiplash injuries. When cervical collars are used as a whiplash injury treatment, there is a 90% probability that you will still have chronic neck pain in six months. Spine, 2000
- One in one hundred people around the world (1% of the population, or just over 70 million people) suffer from ongoing chronic neck pain due to an automobile-induced whiplash injury. Injury, 2005
- One in fifty people injured in Whiplash-like accident deal with chronic pain severe enough to need diagnostic testing, medications, and doctor visits, on an ongoing basis —– nearly eight years after the accident occured. Pain, 1994
“Statistically, every American can expect to be in a motor vehicle collision once every ten years. Motor vehicle collisions have been the number one cause of death of our children for decades. Since 9/11 (September 11, 2001), about 3,000 Americans have died as a consequence of terrorism; about 360,000 Americans have died in motor vehicle crashes. Since the start of the American Revolution in 1775, about a million Americans have died in our wars. Since Henry Ford introduced the mass-produced motorcar in 1913, more than 2.5 million Americans have met their deaths on the road. And millions of Americans who did not die from motor vehicle collisions were injured.” Orthopedist and one of the world’s foremost experts on whiplash, Dr. Dan Murphy. There are 3,000,000 new cases of whiplash in the US every year.
Whiplash Injuries Explained
The word “whiplash” is a layperson’s term —- and although it is typically associated with Car Crashes, crashes are certainly not the only way to get a whiplash injury. Whiplash Associated Disorders (WAD) are typically referred to in the medico-legal literature as “Acceleration / Deceleration” injuries, or “Hyperflexion / Hyperextension” injuries. And, as many of you have come to understand the hard way, they can be incredibly violent — even in seemingly minor accidents that had surprisingly little vehicular damage. With over three million new cases of Acceleration / Deceleration injuries occurring each year, and over 50% of those progressing to at least some degree of unresolved or “chronic” symptoms, it is clear that Whiplash Associated Disorders are taking a massive toll on our country financially, physically, and emotionally.
When people think of “whiplash” they tend to think of motor vehicle accidents (MVA’s). Although MVA is probably the single most common cause of the symptoms most frequently associated with and experienced by those suffering with Whiplash Associated Disorders (neck pain, upper back pain, shoulder pain, fuzzy thinking, numbness, tingling and / or weakness of the hands, dizziness, etc), whiplash can occur in about a thousand and one different ways. And while there are certain symptoms that we see over and over and over in our clinic (neck pain and headaches, for instance), whiplash can seemingly cause about a thousand and one different symptoms as well. Some of the most common causes of WAD that I see in my office include sports injuries, work injuries (think logging here), spousal abuse, fights, horse accidents (falls), and almost anything else that has the capacity to “snap” your head suddenly and violently.
Although the most common problems associated with Whiplash Associated Disorders are related to the neck (neck pain, numb hands, headaches), scientific research shows that Acceleration / Deceleration injuries routinely cause all sorts of other injuries as well. For instance, I commonly see people whose low back pain started with an MVA. I even see people whose FIBROMYALGIA was brought on by the emotional and physical stress of an MVA! One of the most shocking conclusions concerning Whiplash Associated Disorders, was written by a pair of the most well known whiplash researchers on the planet — medical researchers, not chiropractic researchers. Drs. Gargan & Bannister stated in a study that was done in the 1990?s, that whiplash-like injuries frequently result in a whole host of, “bizarre and seemingly unrelated symptoms“. Although there are plenty of malingerers, fakers, scam artists, money-grubbers, and drug seekers out there; far too many people are lumped into these categories simply because their problems do not show up on traditional medical tests such as MRI / CT.
Even though there are literally scores of scientific studies concluding that Whiplash Associated Disorders are difficult (often to the point of being impossible) to image on x-rays, CT’s, or MRI’s, these are still the chief method the medical community is using to determine whether or not you were injured, and just how serious this injury might be. The problem is, if the vast majority of soft-tissue injuries (injuries to LIGAMENTS, TENDONS, MUSCLES, FASCIA, etc) do not image well with advanced imaging techniques, and imaging is the medical community’s chief method of diagnosis; unless you have a herniated disc, you will invariably be treated like nothing is really wrong with you — like you are a scam artist trying to extort a huge settlement from an insurance company. Stop and think for a moment about how problematic that fascia, arguably the single most pain-sensitive tissue in your entire body, will not show up on any tests —- including MRI.
When you are taken the the ER, you will have some tests run and the doctor will look at you and say, “Thank God Mrs. Smith. Nothing is broken! Now, go home and rest, and call your family doctor tomorrow. In the mean time, wear this collar, and take these Anti-Inflammatory Medications, pain pills, and muscle relaxers. Oh, and don’t forget to use a heat pack as well.“ Is this good advice? Sure it is — if you own a medical clinic! Follow this advice and you are certain to become a lifetime ARTHRITIC! The truth is, when it comes to the evaluation and treatment of injuries to fascia and other elastic, collagen-based connective tissues, all of our hi-tech equipment with its bells and whistles is simply not helping diagnose or help most injured people. You are reading a page on whiplash —- my guess is that you completely understand this concept because you have been there, and done that! The Old Model of tissue injury evaluation and treatment went out the door about 25 years ago. It just seems like no one has remembered to tell treating physicians about the NEW MODEL.
Brain Based Injury
Your short drive to work was no different than any other day —- until you began slowing down for the school bus stopping in front of you. Just as you’re coming to a complete stop, BAM; your world explodes as someone plows into your car from behind, knocking you into the bus. Turns out the kid driving the full-sized crew cab pickup truck that hit you was texting, and never even hit his brakes. You’re having a hard time remembering exactly what happened. You remember a flash of light and your head being slammed backwards over the top of your headrest. You vaguely recall that your head rocketed forward as you hit the bus — almost hitting the windshield. You step out of your 1997 Toyota Camry to take stock of the situation. There is no blood or guts. In fact, you don’t even have a bruise to show for your trouble. But by the time the State Troopers arrive to work the accident, you not only have a neck pain unlike anything you have ever felt before, you have a banging headache as well. You’re having trouble putting the pieces in order for them. They ask if you need an ambulance, but you do not want to go to the Emergency Room. But a few weeks later, you’re still having trouble with your memory. Work is not going well because on top of the pain and exhaustion (yeah, since the accident you can’t sleep either), everything seems fuzzy, foggy, and hazy. Who would have thought that whiplash could cause these sorts of symptoms —– particularly without any overt / obvious injuries?
Whiplash Injuries are particularly dangerous because they are a common cause of MTBI (Mild Traumatic Brain Injury). MTBI results from the brain bouncing off the inside of the skull during the hyperextension / hyperflexion of the neck. As you can imagine, this damages / destroys nerve cells. Depending on which part of the brain is injured, a person might have problems in some of the following areas…
- Walking / Moving
- Balance
- Coordination
- Strength / Endurance
- Ability to Communicate
- Ability to Understand
- Ability to Think
- Memory
- Strange or Unexplainable Pain Patterns or Symptoms (these are some of the “bizarre and seemingly unrelated symptoms” talked about by whiplash researchers Gargan and Bannister.)
- Altered Psychological Profiles
Because these symptoms are often subtle, not very specific, and do not show up on standard medical tests such as x-rays or MRI’s, it’s common for patients with MTBI not to complain about them — at least initially. For many people it can be embarrassing “complaining” to the chiropractor or doctor about these vague and difficult-to-describe symptoms that have no external findings to relate them to (bruising, abrasions, broken bones, etc). Believe it or not, many patients are relieved to find out that there is a physiological reason that they feel the way they do, and that it is not “all in their head”. The good news is that with the correct kind of care, most of the patients who are struggling with these injuries will recover within a year’s time. But unfortunately, not all do. It is for this group of people that the term MTBI or “Post Concussive Syndrome” is used.
Factors That Worsen Whiplash Injury
The “old” model of whiplash said that WAD was simply caused by stretched or torn tissue, which was solely the result of the head flying around upon impact. That model simply did not explain the injuries being reported in low-speed collisions (15 mph and under). The most current whiplash models shows that a wave is “shot” through the spine upon impact —- quite similar to the wave you create to move the garden hose a couple of feet to the left. This wave, which occurs in a fraction of a second, can tear both connective tissue and nerve tissue microscopically. It also momentarily induces a tremendous amount of pressure in the smallest blood vessels (capillaries) which is known as “blood hammer”. Blood Hammer, FASCIAL TEARING, and subsequent Neurological Damage, helps to explain some of these “bizarre and seemingly unrelated symptoms” that are almost epidemic in those who have suffered whiplash injuries due to MVA’s.
What Can Make Whiplash Injury Worse?
FACTORS THAT POTENTIALLY INCREASE WHIPLASH SEVERITY
- Unaware of approaching impact
- Being Female (less muscle mass)
- Incorrectly positioned headrest (too low)
- Wet, Icy, or Slick roads (or gravel)
- Automatic Transmission
- Your vehicle is small and light or struck by a larger vehicle
- Elderly or arthritic spine (or history of previous whiplash injury)
- Head turned at impact
- Angled or side-impact accidents (rear-enders are particularly bad)
FACTORS THAT POTENTIALLY DECREASE WHIPLASH SEVERITY
- Aware of approaching impact
- Being Male (more muscle mass)
- Headrest positioned at mid-ear
- Dry Pavement
- Manual Transmission
- Your vehicle is large, heavy, or struck by a much smaller vehicle
- Younger or more flexible and healthy spine (no previous injury)
- Head facing forward at impact
- Straight impacts
Relationship: Severity Of Injury & Amount Of Vehicle Damage
 “Different parts of the human body have different inertial masses. The mechanism of injury from a rear-end motor vehicle collision, is, as a rule, an inertial injury. This means the injury does not occur as a consequence of direct contact of vehicle parts to the patient’s body; rather, injury occurs as a consequence of different inertial masses moving independently from one another.” Dr. Daniel Murphy, Board Certified Orthopedist and Leading Expert in Whiplash Diagnosis and Treatment
“Different parts of the human body have different inertial masses. The mechanism of injury from a rear-end motor vehicle collision, is, as a rule, an inertial injury. This means the injury does not occur as a consequence of direct contact of vehicle parts to the patient’s body; rather, injury occurs as a consequence of different inertial masses moving independently from one another.” Dr. Daniel Murphy, Board Certified Orthopedist and Leading Expert in Whiplash Diagnosis and Treatment
In 1687, famed astronomer / mathematician / physicist / philosopher / and theologian, Sir Issac Newton, wrote his still-renowned Philosophiae Naturalis Principia Mathmatica (now referred to as Principia or simply “Principles”), that is still considered to be the greatest scientific textbook in human history.
In Principia, Newton laid out his three Laws of Motion. These laws are able to explain whiplash and the subsequent injury that follows better than anything else I have seen thus far. For understanding whiplash injuries and their relationship to vehicle damage, Newton’s first law is the most important —- The Law of Inertia. Channel your 8th grade science class and stay with me here as we take a brief science / physics review. Newton’s First Law: Objects at rest remain at rest unless they are acted on by an outside force. Likewise, objects in motion stay in motion unless they are acted on by an outside force. And remember this; Like Dr. Murphy described above, whiplash injuries occur because different parts of your body can and will have different inertias — sometimes very different inertias.
Let’s say that you are sitting at a stoplight and minding your own business. You’re humming along to Manfred Mann’s Blinded by the Light, when all of a sudden —- BAM! You are slammed from behind and launched across the intersection like you were shot from a cannon! You are not sure what happened, but you feel like you just got knocked into next week. PHYSICS LESSON: When your vehicle was struck from behind, it shot forward. Much of this had to do with the fact that you were driving a 1992 Toyota Corolla, and the kid that hit you (he was texting of course) was headed to the sale barn for his dad, driving a F-350 Supercab, and pulling a stock trailer loaded with eight steers. When he hit you, there was a huge instantaneous change in momentum. In a fraction of a second, your Corolla was accelerated from zero to over 50 mph. Let’s look at this event in frame-by-frame fashion.
As the Corolla shot forward, so did your torso that was sitting in the seat. Follow me, because here is the precise point where whiplash occurs. As your body was accelerated forward, your head (at least in the initial milliseconds) did not move. The head is much smaller (and lighter) than your torso, and attached by a thin column of muscles, tissues, and tiny vertebrate we call the neck or Cervical Spine. Because of the weight difference between the head and the body, as well as the fact that the connector between them (the neck) is stretchy and relatively thin; the head has a completely different inertia than the body. This was magnified by the fact that the seat back kept your torso from moving very far backwards, but did nothing to stop your neck — and unfortunately, your head restraint was not adjusted to the proper height. In other words, your body was essentially driven out from under your head; then a fraction of a second later, your head not only caught up with your body, it actually accelerated to a greater velocity than your body, and overshot it as your head slammed forward.
Let’s review: As the vehicle, the seat, and your body rocketed forward with the explosive energy and momentum shift from the impact, your head remained stationary for a split second. Your body was essentially driven out from under your head, making it appear that your head slammed backwards. As your head’s momentum began catch up to that of your body, the tissues in your neck began to stretch and deform. Unfortunately, when the force of the accident is greater than the forces holding your tissues together, these tissues begin to tear —- at least on a microscopic basis (remember, most of the time this tearing and SCAR TISSUE will not show up on an MRI). The result was a whiplash injury —- an inertial injury to the SPINAL LIGAMENTS, SPINAL DISCS, FASCIA, TENDONS, and other soft tissues of the neck and upper back. In fact, there are studies showing that even though they are too small to be effectively imaged with current MRI technology, there are often (usually) microscopic fractures of the FACET JOINTS present with intense whiplash injuries. Frequently, there is also sub-clinical brain injury as well.
Interestingly enough, one of the things that make muscles contract with greater intensity is to maximally stretch them (think of the windup and cocked arm of a baseball pitcher here). When the neck is stretched to such a great degree, it’s muscles contract to an equally intense degree. When coupled with the acceleration and subsequent deceleration of the vehicle, this causes the neck to slam forward causing still more tissue tearing in the neck and upper back. And the most important thing to grasp is that your neck and head never hit anything throughout the entire process. The injury to the neck itself (which happened in a matter of milliseconds) occurred because of a huge momentary shift in momentum, energy, and inertia between your body and your head —- just like what you see in Shaken Baby Syndrome.
Although you are slightly dazed, you get out of your Corolla and begin to appraise the situation. You look at your limbs. They look intact. You can move. You are breathing. There’s no blood. Nothing looks bruised or feels broken. In fact, you do not have as much as a scratch on you. You do not want to go to the Emergency Room, but the State Trooper working the accident talks you in to it. You have several spinal x-rays and a CT of your neck. Everything is negative. The ER doctor comes in, pokes you, prods you a couple times, and has you move a bit. He then delivers a short monologue — one he has delivered hundreds of times previously, “Wow Mr. Jones. Sounds like you were born under a lucky star. Thank God nothing is broken. Neurologically you check out fine. You’ll be sore, but just go see your family doctor tomorrow. You’ll get some PAIN PILLS, NSAIDS, CORTICOSTEROIDS, and MUSCLE RELAXERS. Don’t worry. You’ll be just fine.”
But that’s just it. You saw your doctor, and as the weeks go by, you’re not fine. Far from it. You are in pain, and it’s getting worse. But you have nothing to show for it. Like I said, there were no broken bones and no bruises. Heck, there was not even a cut or scratch. There is nothing that would alert anyone (let alone a doctor who is not up on the most current research) that you are in pain —- and that it’s getting worse. And on top of that, the damage to the rear end of your Corolla looked surprisingly light compared to how hard you were hit and the way that you feel (for Pete’s sake, the car is actually drivable). The other fellow’s insurance company paid you $2,000 for your Toyota, which was over double the Kelly Blue Book value. They took care of the ambulance ride and Emergency Room visit, and even offered you $1,500 for pain and suffering. You hired an attorney, but he acts like he does not really believe how much you hurt either. What’s going on here?
Almost half a century ago (1964), the prestigious medical journal, American Journal of Orthopedics revealed a still well-concealed fact — that there is no relationship (none, nada, zilch, zero) between the damage done to the vehicle and the amount of injury to the vehicle’s occupants. Since that time, the medical and scientific communities have proved this fact over and over and over again via research. It is a fact that I have heard verified over and over and over again by the Law Enforcement Officers and Paramedics that I adjust on a regular basis. Although most of the time, Insurance Companies and the Attorneys that represent them would have you believe just the opposite (there was not enough vehicle damage to have an injury), it’s just not true. Decades worth of scientific studies tell us that the severity of the vehicle damage cannot predict….
- If patients will suffer whiplash injuries.
- How severe those injuries might be.
- How long it will take to effectively treat / heal the injury — or whether they will ever really heal at all.
- Whether or not the injured party will end up with Chronic Pain and / or Arthritis as a direct result of the accident.
Dozens upon dozens of studies on Motor Vehicle Accidents have shown that vehicles that do not crumple upon impact will be accelerated with a far greater force and momentum. The faster that your vehicle is accelerated upon impact, the greater the inertial stresses to the neck and upper back. This is why today’s vehicles are made with “crumple zones”. You are much better off if the force of impact is absorbed by vehicular deformation, than by deformation of your body, particularly the soft tissues and discs of your neck. The larger the inertial stresses to the neck and upper back, the greater the damage to the soft tissues of the cervical spine / neck.
So, it stands to reason that harder impacts and greater amounts of vehicle damage lead to greater amounts of bodily injury. Not only is this not true, but most of the medical research on whiplash injuries today is being done on the effects of low speed impacts (those under 15 mph). Here are a few of the Scientific / Medical / Legal profession’s journals saying that there is no relationship between the amount of vehicular damage and the amount of injury to the vehicle’s occupants.
- The Spine, 1982
- Orthopedic Clinics of North America, 1988
- Society of Automotive Engineers, 1990
- Injury, 1993
- Trial Talk, 1993
- Injury, 1994
- American Journal of Pain Management, 1994
- Society of Automotive Engineers, 1995
- Society of Automotive Engineers, 1997
- Archives of Physical Medicine and Rehabilitation, 1998
- Journal Of Whiplash & Related Disorders, 2002
- Spine, 2004
- Journal of Neurology, Neurosurgery, and Psychiatry, 2005
- Spine, 2005
- Whiplash Injuries, 2006
One of the problems, however, with whiplash injuries is that they frequently end up causing DEGENERATIVE ARTHRITIS. This has to do with the fact that these inertial injuries damage tissues in ways that cannot be imaged using even the most advanced technologies. Because most doctors are not up on current whiplash research, and feel you are looking for a big settlement, they frequently treat you like a malingerer (faker). However, these injuries cause the microscopic fibrosis that causes abnormal joint motion over time. This leads to arthritis so frequently, that I can often predict with a great deal of accuracy when a person’s injury occurred — just by looking at a current x-ray of their neck.
Arthritis After An Automobile Accident
- X-rays taken an average of seven years after a whiplash injury revealed that arthritis in the neck’s spinal discs in almost 40% of the patients. The study’s uninjured group showed only a 6% rate of arthritis. What did the authors conclude? “Thus, it appeared that the injury had started the slow process of disc degeneration.” The Cervical Spine Research Society, 1989
- Whiplash patients who already had degenerative arthritis of their cervical spine (neck), showed evidence of degenerative arthritis at previously non-arthritic discs and vertebrates in 55% of cases. The Cervical Spine Research Society, 1989
- Compared to the necks of uninjured patients, a single incidence of whiplash increases the occurance of neck arthritis by 10 years. The Journal of Orthopedic Medicine, 1997
- Pre-exisiting arthritis of the neck / Cervical Spine, greatly worsens the effects of a whiplash injury. Numerous studies show how this slows recovery times and increases the probability of ending up with Chronic Pain and even more arthritis than you started with. British Journal of Bone and Joint Surgery, 1983; The American Academy of Orthopedic Surgeons, 1987; Orthopedic Clinics of North America, 1988; Spine, 1994; British Journal of Bone and Joint Surgery, 1996
- A great example of Inertia Injuries involves the sport of soccer. Soccer players who regularly “head” soccer balls, speed up degenerative arthritis of the neck by as much as twenty years. European Spine Journal, 2004 This is not new information, however. I wrote a newspaper column on the subject clear back in 1993. We saw that professional soccer players had double the amount of neck arthritis as their non-soccer playing peer group.
Whiplash Disorders: Difficult To Diagnose Despite Advanced Imaging
WAD is difficult to properly diagnose or evaluate using standard medical tests. X-rays do not ever show soft connective tissues, and dozens of studies show that MRIs, contrary to popular belief, do a poor job of imaging injured soft tissues — ESPECIALLY FASCIA. This is why you might feel like you are “dying”, but all of the tests are negative. People go through this experience over and over. They are then sent home from the E.R. or doctor’s office with pain killers, muscle-relaxers, and anti-inflammation drugs which can actually cause injured tissue to heal approximately 1/3 weaker and less elastic than it otherwise would, and told that in time it will heal. Just like a broken arm that is cocked off at a funny angle but never set or put in a cast; it will heal….. It just won’t heal the right way or with the proper amount of joint function / motion.
So just how should a problem like this be addressed? The key to a functional recovery is controlled motion. CHIROPRACTIC ADJUSTMENTS, specific stretches, and strengthening exercises are the number one way to accomplish this! Because FASCIAL ADHESIONS are usually part of the whiplash equation, you will probably need to undergo some form of Tissue Remodeling as well. Restoring movement, function, and strength (both to individual joints or vertebrate, and to the spine or limb as a whole) is the only proven method that is effective in truly reducing the symptoms of whiplash. Contrary to popular belief, using drugs to simply cover symptoms, is never a good option.
If the only treatment you receive for your whiplash injury is palliative (meaning covering symptoms with drugs, without addressing the underlying cause of those symptoms), then any relief achieved is temporary, and the end product of this process will likely be dysfunction, degeneration, and chronic pain!
Doctor/s Cannot Find Anything Wrong: What To Do

I would seriously consider getting a new doctor. As you have already read, whiplash is frequently a “clinical” diagnosis. This simply means that it is not going to show up well on standard imaging tests such as x-rays, CT, and even MRI. If your doctor is not up on the most current whiplash research, you lose — in more ways than one. Let me show you the results of one study that wanted to determine if the effects of whiplash were real (“organic”) or in the patient’s head (“psychometric”). By the way, this study comes from a 1997 issue of one of the planet’s most prestigious medical journals, The Journal of Orthopedic Medicine. They compared a large control group to a large whiplash group, ten years after the accident. Not only does this give us a long-term look at the effects of whiplash, it also removes the potential effects of litigation on the research as any legal issues would have been long settled.
NON-WHIPLASH INJURED GROUP
- Neck Pain
- Headaches
- Numbness, Tingling, Pain, Paresthesia in Arms / Hands
- Combined Back and Neck Pain
- Neck Degeneration as Seen on X-rays
WHIPLASH INJURED GROUP
- Eight Times more Neck Pain
- Eleven Times more Headaches
- Sixteen Times more Numbness, Tingling, Pain, Paresthesia in Arms / Hands
- Thirty Two Times more Combined Back and Neck Pain
- Neck Degeneration was Ten Years Advanced when Compared to the Control Group
Hyperflexion/Hyperextension Of The Cervical Spine
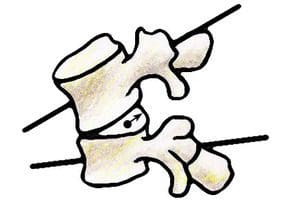
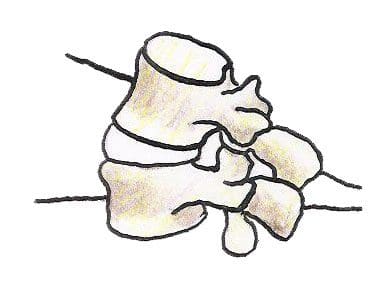
 With Hyperflexion, the spine goes forward, which drives the Nucleus of the disc to the back. This is why Herniated Discs are a frequent result of Whiplash Injuries. In Hyperextension, the spine is slammed backward. Although this rarely if ever results in frontal Disc Herniations, it jams the facets (the two little joints to the rear and on either side of the disc). This can lead to a degenerative condition called Facet Syndrome.
With Hyperflexion, the spine goes forward, which drives the Nucleus of the disc to the back. This is why Herniated Discs are a frequent result of Whiplash Injuries. In Hyperextension, the spine is slammed backward. Although this rarely if ever results in frontal Disc Herniations, it jams the facets (the two little joints to the rear and on either side of the disc). This can lead to a degenerative condition called Facet Syndrome.
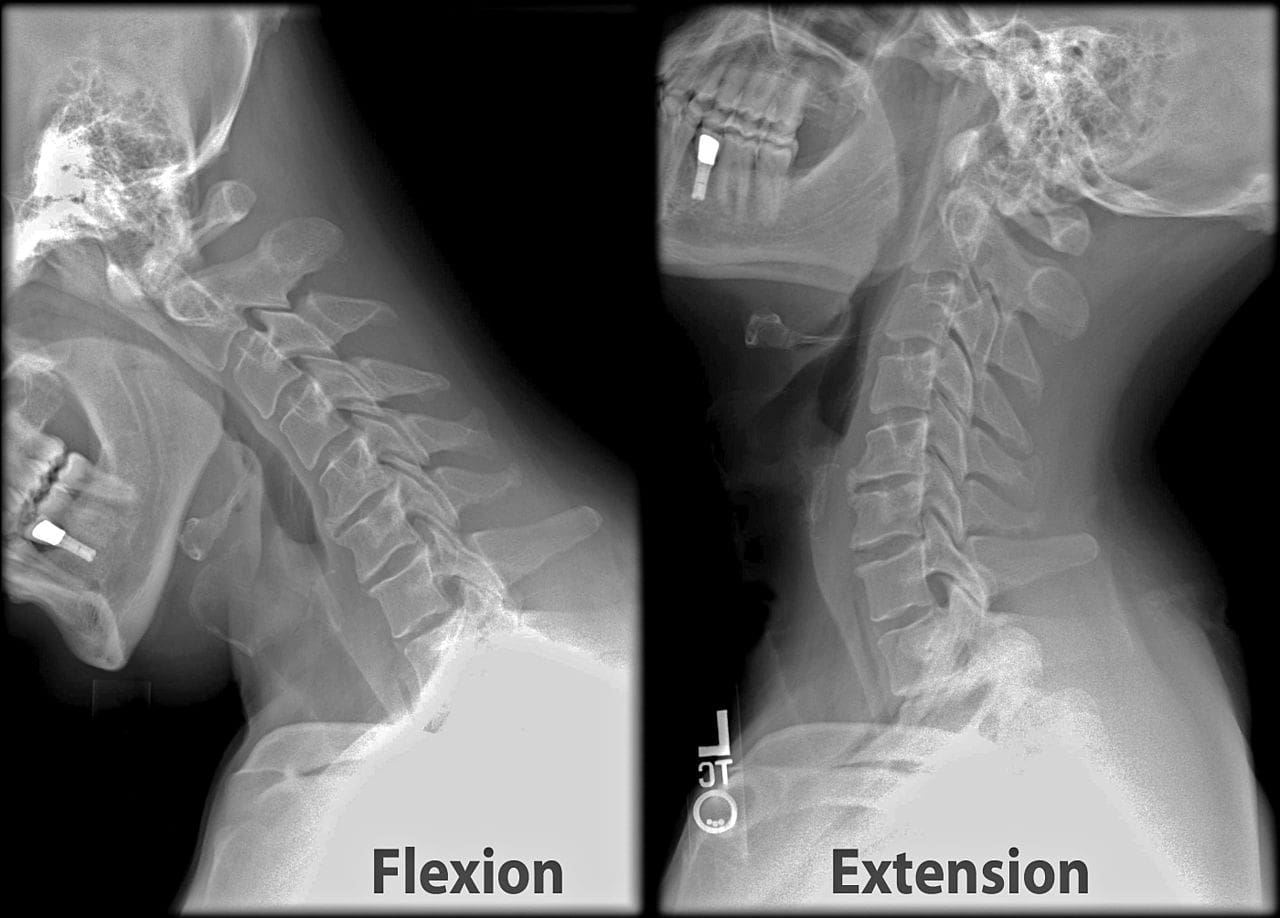
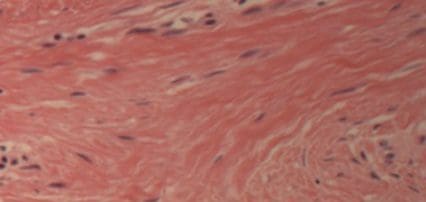
Notice in this Flexion / Extension X-ray that there is Spinal Degeneration occurring at the level of the C5-C6 Spinal Disc. This means that either this X-ray is being taken years (maybe decades) after an injury, or that this person had pre-existing degeneration (bone spurs, thin discs, and calcium deposits) prior to this latest injury. Either way, the individual being X-rayed had a Flexion / Extension injury of some sort probably 20 years ago or so. How can we predict this. Although there is a certain degree of “guesswork” that goes into knowing this, we know that DEGENERATIVE ARTHRITIS occurs due to loss of joint motion over time, and that whiplash tends to strike worst at C5-C6.
Soft Tissue Injuries?: How Long Do They Take To Heal?
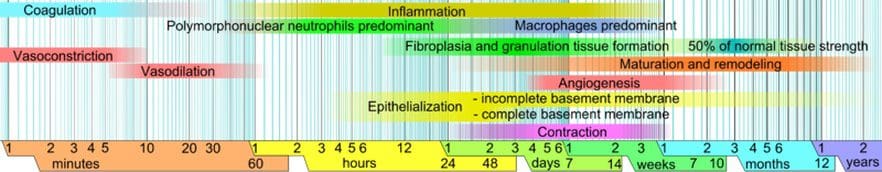
For people injured in Automobile Accidents, falls, Horse Accidents, Motorcycle Crashes, or any number of other ways that people end up with “Whiplash Injuries”, this is a commonly-asked question. But it’s also a commonly asked question for those whose soft tissue injury was not traumatic, but was due to chronic, repeated, sub-maximal loading. It’s more than understandable. No matter how the injury occurred or what it is, everyone wants to know how long it is going to take to get better. Just bear in mind that healing takes time. And although you will often hear “6-8 weeks” bantered around, this is only partially true. If you will notice the chart below, you can see that after about 3-4 weeks, the only thing going on is “Maturation and Remodeling”. Do not be fooled! This phase is not only critical, but far too often ignored by those who have a financial interest in your injury.
Tissue Repair & Healing Phases
STAGE I (Inflammatory Phase): This phase lasts from 12-72 hours, and is characterized by a release of inflammatory chemicals by injured cells. When cells are injured and die, they rupture and release their contents into the extracellular fluid (WHAT IS INFLAMMATION). These “Inflammatory Chemicals” that are released from ruptured cells are a necessary and vital component of the healing process. However, in excessive amounts, they can cause a great deal of pain. They also promote excessive microscopic scarring. Be aware that if you visit your doctor for a soft tissue injury, you will be given anti-inflammatory medications. These have serious side-effects (heart, liver, kidneys, etc). However, the real kick in the teeth is the fact that this class of drug has been scientifically proven to cause injured connective tissues to heal significantly weaker and with less elasticity than they otherwise would. Nowhere is this more true tha with Corticosteroids. Do a quick search of the Medico-Scientific Literature on Corticosteroids and soft tissue injuries. You will see over and over again that they are detrimental to the healing process and should play no part in the treatment of these injuries (HERE is an example from the field of Sports Injuries).
STAGE II (Passive Congestion): In this phase that begins by the 2nd to 4th day, we begin to see swelling (sometimes we do not see it, because it is not on the body’s surface). Remember; “inflammation” is not synonymous with swelling. Inflammatory Chemicals released by dying cells attract the fluid that causes swelling. This is why using cold therapy (ice) to control both inflammation and swelling is such an important part of the healing process — particularly in its earliest stages. However, the best method for moving out this “Congestive Swelling” is via controlled motion if possible. Oh, and your doctor may tell you to use heat during these initial two phases of soft tissue healing; don’t do it. Use ICE to control the inflammation!
STAGE III (Regeneration & Repair Phase): The Repair Phase is where new collagen fibers are made by fibroblasts. The body then uses these collagen fibers as a sort of soft tissue “patch”. Just like with your old blue jeans, a patch is not ideal. But once those old Levis tear or rip, what else are you going to do? In the body, this collagen patch (scar tissue) tends to be different than the tissue around it in a number of ways. Scar Tissue is weaker, less elastic, MUCH MORE PAIN SENSITIVE, has SEVERELY DIMINISHED PROPRIOCEPTIVE ABILITIES, etc). Be aware that the Repair Phase of tissue healing only lasts about 6 weeks, with the majority being completed in half that time. WARNING: This 3rd stage of healing is where many of the so-called “experts” want you to believe the process of Tissue Healing & Repair ends because this phase ends within a month of injury. But that’s not where the story ends. Dr. Dan Murphy uses dozens of studies to, “document that the best management of soft tissue injuries during this phase of healing is early, persistent, controlled mobilization. In contrast, immobilization is harmful, leading to increased risk of slowed healing and chronicity”.
STAGE IV (Maturation / Remodeling Phase): Not only is it the longest, but the Remodeling Phase is by far the most critical of the four stages of Connective Tissue healing. Yet it is the phase that most often gets overlooked. It is also where people most often get duped (sometimes inadvertently, but more often than not, purposefully) by doctors, insurance companies, and attorneys. Many of you reading this know exactly what I am talking about. The most current research shows that in case of serious Connective Tissue Injury, the Remodeling Phase can last up to two years; making the old “6-8 weeks” sound ridiculous (gulp)! The Remodeling Phase is characterized by a “realignment” (REMODELING) of the individual fibers that make up the injured tissue (the collagen “patch” that we call Scar Tissue). What is interesting is that each study that comes out on this topic, seems to be saying that this phase of healing lasts longer than what the study that came out before it said. This is a good thing. However, bear in mind that if you have not improved within 90 days after injury, standard forms of treatment become much less likely to help you. Phase IV can also be risky because although a person’s pain may have dissipated, the injury itself has not completely healed and is vulnerable to re-injury.
As Controlled Loading / Tensile Loading is applied to the healing tissues via CHIROPRACTIC ADJUSTMENTS, Scar Tissue Remodeling, STRETCHING and strengthening exercises, Proprioceptive Re-education, Massage Therapy, TRIGGER POINT THERAPY, PNF, etc; the individual tissue fibers move from a more random, tangled, and twisted wad of unorganized collagen fibrils; to a tissue that is much more organized, parallel, and orderly as far as its microscopic configuration is concerned. Again, this takes time! Although our Scar Tissue Remodeling Therapy can frequently bring immediate relief (just look at our VIDEO TESTIMONIALS), it is obvious from the medical literature that there is a healing processes that cannot be bypassed. Because numerous Scientific Studies have proved Cold Laser Therapy to be effective in regenerating Collagen (SEE HERE), we highly recommend it for our more seriously injured patients as well.
Everyone has heard the old cliche that is still used by doctors, “You’d have been better off to break the bone than to tear the ligaments”. Knowing what we know about the healing of the Collagen-Based, Elastic Connective Tissues; this statement makes a lot of sense! Soft tissues heal much slower than other tissues (including bones). Do not let anyone try and convince you otherwise! This is why following the complete stretching and strengthening protocol that goes hand-in-hand with our “Tissue Remodeling” treatment, is the one and only way that it will work properly over the long haul. By the way, we have dealt extensively with the fact that whiplash injuries heal best with forms of therapy that employ controlled motion such as does chiropractic. Now I want to explore what the scientific literature says about using medications for whiplash injuries explained.
Whiplash Injuries Explained: Relationship Of Inflammation To Pain & Scar Tissue
In 2007, the renowned pain researcher Dr. Sota Omoigui, published an article in the medical journal Medical Hypothesis called, “The Biochemical Origin of Pain: The Origin of All Pain is Inflammation and the Inflammatory Response”. In it, he showed the relationship between pain, inflammation, and fibrosis (Scar Tissue). Most people tend to think of Inflammation as a “local” phenomenon. You know; sprain an ankle, and it swells — sometimes a whole bunch. But it is critical to remember that the terms “swelling” and “inflammation” are in no ways synonymous. When cells of soft tissues are seriously injured (like in Whiplash Injuries), they die. These dead then rupture their contents into the surrounding extra-cellular fluid. In response to this, the Immune System makes a group of chemicals that we collectively refer to as “Inflammation”, which in small amounts, are normal and good. Their local presence is indicated by five well known signs and symptoms. The classical names for the various signs of Local Inflammation come from Latin and include:
- Dolar (Pain)
- Calor (Heat)
- Rubor (Redness)
- Tumor (Swelling) Chemicals we collectively call “Inflammation” are not synonymous with swelling, but they attract swelling.
- Functio Laesa (Loss of Function)
Although these chemicals can remain in a local area (I stub my toe, the toe gets red and inflamed), they can invade the blood stream and have a systemic (whole body) effect as well. But inflammation does not end there. These immune system chemicals that we refer to collectively as “inflammation” (prostaglandins, leukotrienes, thromboxanes, cytokines, chemokines, certain enzymes, kinnins, histamines, eicosanoids, substance P, and dozens of others) are being touted by the medical community as the primary cause of a whole host of physical ailments, when there are too many of them in the body. Some of the other problems that Inflammation is known to cause includes;
- Disc Injuries, Slipped Disc, Disc Herniation, and Disc Rupture
- Heart Disease and virtually all forms of Cardiovascular Problems
- Skin conditions including Eczema and Psoriasis
- Arthritis & Fibromyalgia
- Asthma
- ADD, ADHD, Depression, and various forms of Dementia
- Neurological Conditions
- Female Issues
- Cancer
- Inflammatory Bowel Disease / Leaky Gut Syndrome
- Diabetes, Insulin Resistance, Hypoglycemia, and other Blood Sugar Regulation Problems
- Obesity
Inflammation causes pain, ill health, and eventually, death. But this list is not the thrust of this section. To understand is the way that inflammation is related to Scar Tissue, Adhesion, and Fibrosis.
Born in 1904, Dr. James Cyriax, a Cambridge-educated M.D. widely known as the “The Einstein of Physical Medicine” wrote his Magnum Opus, Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions, in 1982 shortly before he passed away. Cyriax is still considered one of the brilliant pioneers of soft tissue research. One of Dr. Cyriax’ groundbreaking discoveries is that Scar Tissue / Fibrosis can and will generate an Inflammatory Response long after the Fourth Stage of Healing (Maturation & Remodeling) is over. Pay attention to what Cyriax wrote over three decades ago.
“Fibrous tissue appears capable of maintaining an inflammation, originally traumatic, as the result of a habit continuing long after the cause has ceased to operate…… It seems that the inflammatory reaction at the injured fibers continues, not merely during the period of healing, but for an indefinite period of time afterwards, maintained by the normal stresses to which such tissues are subject.”
Why would what Cyriax refers to as “normal mechanical stresses” cause an “indefinite period” of inflammation? This one is easy. Scar Tissue and Fibrosis are so dramatically different from normal tissue. One of the most obvious ways that this can be seen is by looking at any good Pathology Textbook. Scar Tissue and Fibrosis is far weaker and much less elastic than normal Connective Tissue. What does this mean? Only that it is easily re-injured. This starts the whole vicious cycle over again. Injury —-> Inflammation —> Pain —> Fibrosis & Scar Tissue Formation —> Re-injury —> Repeat indefinitely. Just remember that the end result of this cycle is degeneration of the affected bones and spinal discs!
Notice how the Connective Tissue on the left is uniformly wavy. This is due to the collagen fibrils that provide stretchiness and elasticity. Now notice how the cells of the Scar Tissue and Fibrosis run and swirl in many different ways. This decreases both elasticity and strength of the Scar Tissue.
Scar Tissue & Fibrosis: Different From Normal Tissue, 3 Ways
SCAR TISSUE IS WEAKER
Repaired soft tissues are weaker than the body’s undamaged soft tissues. The diameter of the collagen fibers of scar tissue are smaller than those of normal tissue. Also, as you can see from the pictures above, the structure has been physically changed. This weakness leads to a viscous cycle of instability, re-injury, and degeneration.
SCAR TISSUE IS LESS ELASTIC
Repaired soft tissues are always less elastic and “stiffer” than the body’s undamaged soft tissues. This has to do with the fact that the individual collagen fibers will never identically align themselves quite like the original uninjured soft tissue. This is all easy to see because range of motion testing on injured individuals will always show areas of decreased ranges of motion.
SCAR TISSUE IS MORE PAIN-SENSITIVE
Repaired soft tissues have a strong tendency to be more pain-sensitive than their uninjured counterparts. In fact, for reasons that are not completely understood, Scar Tissue has the neurological capability of going into something called “super-sensitivity”, and can end up 1,000 times more sensitive to pain than normal tissue.
Relationship: Inflammation, Pain, & Fibrosis/Scar Tissue
Dr. Soto Omoigui had this to say about the relationship between pain, inflammation, and fibrosis, “The origin of all pain is inflammation and the inflammatory response…. Irrespective of the type of pain, whether it is acute or chronic pain, peripheral or central pain, nociceptive or neuropathic pain, sharp, dull, aching, burning, stabbing, numbing or tingling, the underlying origin is inflammation and the inflammatory response.” Fellow pain researcher Doctor Manjo stated in the “Chronic Inflammation” chapter of his 2004 pathology textbook that (slightly paraphrased for patients), “After a day or two of acute inflammation, the connective tissue—in which the inflammatory reaction is unfolding—begins to react, producing more fibroblasts, more capillaries, more cells—more tissue, but it cannot be mistaken for normal connective tissue. Fibrosis means an excess of fibrous connective tissue. It implies an excess of collagen fibers. When fibrosis develops in the course of inflammation it may contribute to the healing process. By contrast, an excessive or inappropriate stimulus can produce severe fibrosis and impair function. Why does fibrosis develop? In most cases the beginning clearly involves chronic inflammation. Fibrosis is largely secondary to inflammation.”
It is not difficult to connect the dots! Chronic Inflammation of a whiplash injury leads to Scar Tissue Formation, and Scar Tissue Formation leads to even more pain. And like I mentioned earlier, the whole mess leads to Spinal Degeneration. How can you break free? Dr. Cyriax goes on to say in his book that immobilization of injured soft tissues is a bad thing, and mobilization of injured soft tissues is not only good, but necessary for proper healing to take place. But under the umbrella of America’s PHARMACEUTICAL DRUG CULTURE, functional restoration frequently takes a back seat to different kinds of medicines. Don’t get me wrong; if you need something for the pain after a whiplash injury, there is no dishonor in doing something on a short-term basis. However, this is never the solution. It is masking symptoms to get you through a rough place. As long as you understand this, OK. However, there is one class of drugs that should play no part in the healing of your Whiplash Injury…
Inflammation Medications For Whiplash & Soft Tissue Injuries
- The most prestigious medical school on the planet, John’s Hopkins proved that 1,000 200 mg capsules of Tylenol consumed over the course of a person’s lifetime doubles that person’s chances of dialysis. Furthermore, 5,000 pills increase kidney failure by nearly nine times. New England Journal of Medicine, 1994
- Regular use of Tylenol and other similar medications is a top cause of liver disease / liver failure. New England Journal of Medicine, 1997
- NSAID’s (Non-Steroidal Anti-Inflammatory Drugs) used by arthritis sufferers causes 16,500 Americans to die of bleeding ulcers each year. Fatal GI bleeds are the 15th most common cause of death in America. New England Journal of Medicine, 1999
- Gastrointestinal (GI) toxicity caused by NSAID use is one of the most commonly seen and serious drug side effects in modern cultures. Spine, 2003 & Surgical Neurology, 2006
Regular use of Tylenol doubles one’s chances of developing high blood pressure. Hypertension, 2005
All NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) increase chances of Myocardial Infarction (heart attack) by about 40%. This risk starts the first day the drug is consumed. European Heart Journal, 2006 - Celebrex increases your chances of intestinal bleeding by four times (nearly 400%). Vioxx increases your chances of bleeding ulcers and other GI Bleeds by over three times (nearly 330%). Medications taken for pain increase your chances of GI Bleeds by nearly 140%. Drug Safety, 2009
- Vioxx was removed from the market in 2004 because it increased one’s chances of a heart attack by 230% (exponentially more if you already had a congestive heart). Celebrex increased the risk of heart attack by 44%. Pain Medications, on average, increase your chances of a heart attack by nearly half 50%. While Vioxx was pulled from the market, the others are considered to be “acceptably safe” and they were allowed to stay on the market. Drug Safety, 2009
- Those who took the greatest amounts of NSAID pain medications increased their chances of all types of dementia —– Alzheimer’s included. The increase was a whopping 2/3 (66%). Neurology, 2009
So, what is a person supposed to do? Despite decades of research saying that NSAID’s are not “therapeutic” (actually helps you get better), but are instead, “palliative” (makes you feel better without any therapeutic benefits), the medical community continues to hand these and other dangerous drugs out almost like candy. Just remember that any pain relief achieved without addressing the underlying components of the Whiplash Injury, are temporary. And that’s not all. When joints and tissues heal in RESTRICTED FASHION, they always end up with copious amounts of decay, degeneration, and deterioration. And the final kick in the teeth for those of you who have been on this MEDICAL MERRY-GO-ROUND is that much of this research is at least two decades old. As I have said for a very long time, much of the medical community is caught in a time warp. They are treating whiplash injuries using outdated models, often times very outdated models.
Chiropractic Benefits: Whiplash, Neck/Back Pain
- Over 70 years ago, the best available research said that soft tissue injuries require early and regular joint motion in order to heal properly. American Journal of Anatomy, 1940
- Over 50 years ago, research pointed out that the most effective treatment for whiplash injury does not involve medication, but instead needs mobilization, manipulation and traction to heal. The best results for patients with whiplash injuries require early and regular joint mobilization. Furthermore, it must be done by someone expertly trained in rehabilitation of injured joints. Journal of the American Medical Association, 1958
- For injured soft tissues to heal properly requires joint movement / motion. Joint immobilization should be avoided. Textbook of Orthopedic Medicine, 1982 & Continuous Passive Motion, 1993
- Chiropractic spinal adjustments fix over 4/5 of disabled patients suffering from chronic low back and sciatica. This is true despite the failure of other approaches. Canadian Family Physician, 1985
- Chiropractic spinal adjustments have been proven superior in the treatment of chronic and acute low back pain, when compared to hospital outpatient treatment. These benefits of chiropractic adjustments were still seen 3 years post-treatment. British Medical Journal, 1991
- Chiropractic spinal adjustments have been shown to be more effective than physical therapy mobilizations and manipulations. Lancet, 1991
- 93% of those struggling with chronic pain due to whiplash injury —- who have already failed medical care and physical therapy —- improve significantly under chiropractic care. Injury, 1996
- When it comes to chronic neck pain, manual manipulation of the neck has been shown to be significantly better than pain meds and exercise. Annals of Internal Medicine, 2002
- Chiropractic spinal adjustments have been clinically proven to be over five times more effective than NSAID’s (Non-steroidal Anti-Inflammatory Drugs) for chronic neck and low back pain. In this study, the chiropractic group suffered from no adverse reactions, but the the NSAID group had more patients reporting adverse drug reactions than were actually helped. Half the NSAIDS used in the study are now off the market. Spine, 2003
- For chronic neck and back pain, chiropractic spinal adjustments proved significantly better than both acupuncture and pain medicines. Furthermore, chiropractic adjustments were the only treatment studied that showed therapeutic benefit one year post-treatment. Journal of Manipulative and Physiological Therapeutics, 2005
- In patients with chronic pain from DEGENERATIVE ARTHRITIS, 59% can eliminate their pain meds by taking omega-3 fatty acids found in fish oil (EPA & DHA). Surgical Neurology, 2006
- In the recent medical publication called, “A Review of the Evidence for the American Pain Society and the American College of Physicians Clinical Practice Guideline”, only spinal manipulation was touted as effective for the treatment of both acute and chronic low back pain. Annals of Internal Medicine, 2007
- A joint research effort from the University of California, San Francisco, and Harvard Medical School, showed that “Chiropractic care is more effective than other modalities for treating low back and neck pain”. Do Chiropractic Services for the Treatment of Low Back and Neck Pain Improve the Value of Health Benefits Plans? An Evidence-Based Assessment of Incremental Impact on Population Health and Total Health Care Spending, 2009
Long Term Prognosis: Whiplash
Despite the fact that you can see from the current scientific literature how successful chiropractic care is at helping people with severe, debilitating, whiplash injuries; not everyone injured in an MVA will recover. Unfortunately, many will never recover —- even after several decades. It seems that whiplash caused by Motor Vehicle Accidents is the portal whereby numerous people enter into the realm of Chronic Pain and dysfunction. The truth is that there is a great deal of scientific research done of this particular topic. And furthermore, as you can see from the small comments in red made by the authors of each individual study, litigation seems to have little or no effect on clinical outcomes.
- The Journal of Bone and Joint Surgery published research in 1964 showing that of 145 patients involved in a study of whiplash injuries; as many as 83% of the injured patients continued to suffer from pain two years after the accident. The study’s authors said this, “If the symptoms resulting from an extension-acceleration injury of the neck are purely the result of litigation neurosis, it is difficult to explain why [at least] 45%of the patients should still have symptoms two years or more after settlement of their court action.”
- A 1989 issue of Neuro-Orthopedics published a study was carried out on patients suffering with whiplash for well over a decade. Despite the length of time involved, nearly two thirds still struggled with moderate to severe pain symptoms due to their accident. The study’s authors said this, “If symptoms were largely due to impending litigation it might be expected that symptoms would improve after settlement of the claim. Our results would seem to discount this theory, with the long-term outcome seeming to be determined before the settlement of compensation.”
- A 7-year study on whiplash-injured patients published in a 2000 issue of the Journal of Clinical Epidemiology showed that 40% of those suffering an accident-induced whiplash injury continued to suffer from neck and shoulder pain seven years post-accident.
- A 2005 research project published in the medical journal Injury, showed that over 20% of those injured in a whiplash injury struggled with Chronic Pain nearly 8 years post-injury. Furthermore, almost half of those in the study suffered from “Nuisance Pain” during the same time frame.
- An 11 year study published in a 1990 issue of the British Journal of Bone and Joint Surgery showed 40% of the whiplash patients struggling with Chronic Pain over a decade after the fact. 40% of the remainder of the study’s people dealt with “Nuisance Pain” during the same period. The study’s authors said this, “The fact that symptoms do not resolve even after a mean 10 years supports the conclusion that litigation does not prolong symptoms.”
- A fifteen and a half year study published in a 1996 issue of the British Journal of Bone and Joint Surgery reported that well over 40% of whiplash-injured patients struggled with Chronic Pain from the accident over a decade and a half after the fact. Almost 30% of the rest dealt with “Nuisance Pain” over the course of the study. The study’s authors said this, “Symptoms did not improve after settlement of litigation, which is consistent with previous published studies”.
- The European Spine Journal published a nearly two decade long study on whiplash-injured patients in 2002. Well over half (55%) of those studied had pain seventeen years post-accident. One quarter of these dealt with daily neck pain, and almost one quarter had radiating arm pain on a daily basis. The study’s authors said this, “It is not likely that the patients exposed to motor vehicle accidents would over-report or simulate their neck complaint at follow-up 17 years after the accident, as all compensation claims will have been settled.”
- In one of the longest studies done to date on whiplash injured patients, a 2006 issue of the British Journal of Bone and Joint Surgery looked at whiplash-injured patients three decades after their initial injury. 15% of these patients struggled with daily pain severe enough to require treatment. Four out of ten of the remainder dealt with “Nuisance Pain” over the same time frame.
Attorney’s, Insurance, Fees & Medical Pay
After 20 years of practice, I can almost say that I have seen it all. Almost. One thing that I have not seen is an improvement in the way that the financial responsibility for Motor Vehicle Accidents (MVA) is handled by insurance companies. This is a big part of the reason that I do not accept automobile insurance (yours or the other party’s) for the treatment of injuries sustained in MVA’s. Attorneys tend to get involved, and I have found that in most cases, attorneys don’t really work for you, they work for themselves.
WHERE DOES THIS ALL LEAD?
Although, I do not treat huge numbers of MVA cases acutely (they tend to go wherever their attorney sends them usually whoever can run up the highest bills), I treat scores of MVA victims once they have reached the chronic stage. After their attorney reaches a settlement for their injured client, any treatment they were receiving typically ends. As you can tell from both our Patient Testimonial Page, as well as our Blog Post called the WEEKLY TREATMENT DIARY, the treatment frequently ends without ever effectively dealing with the underlying scar tissue and Fibrotic Adhesions that leave so many people in Chronic Pain, long after they have settled their injury claim.
These folks enter the miserable world of CHRONIC NECK / BACK PAIN and HEADACHES, and then wonder what the heck they are going to do because their $3,000 settlement check is long gone. The patient is then left with a choice. They can climb back on the Medical Merry-Go-Round and continue to spin in circles. Tests, blood work, MRI’s, CT scans, drugs, drugs, and more drugs; and therapy — more of the same (expensive) stuff you went through before you settled your case, with more of the same crappy results. Or they can do something different.
Prevent Whiplash Injuries & Lessen The Effects

There are several ways to go about preventing or at the very least, lessening the potential effects of a whiplash-like accident / injury. one of the most effective would be driving a vehicle that is highly rated in crash tests. What is the safest vehicle on the road today? Without a doubt, the Volvo and Saab brands have out-performed every other auto maker in the market today as far as safety is concerned. However, there are a number of things you can do to protect yourself besides trading your Chevy in for a Volvo.
- DRIVE A SAFE VEHICLE: Make sure that the vehicle you drive is highly rated by the organizations that rank automobile safety. This information can be found HERE.
- DRIVE SAFELY AND DEFENSIVELY: This is common sense. Because I rode a motorcycle for many years, I learned how to drive defensively. I always thought that by paying attention and trying to think one step ahead of everything going on around me, crashes with other vehicles could be avoided. That was until I hit a drunk who ran a stop sign (I was in a full-sized Chevy Silverado). Things happen quickly, that you have no control over. However, driving your automobile in an unsafe manner definitely puts you at a higher risk for suffering a Whiplash Injury.
- WEAR YOUR SEAT BELTS: The simple truth of the matter is that seat belts will probably not lessen the “Whiplash” component of an Automobile Accident. In fact, by holding your body in place while your head flies around, they can potentially worsen a neck injury to the soft tissues. However, seat belts will help to keep you alive.
- MAKE SURE YOUR HEAD RESTRAINT IS ADJUSTED PROPERLY: This is by far the most important thing you can do diminish your chances of Whiplash Injury should you end up in an MVA. The truth is, most of us refer to these things that stick out of the top of our seats as “Head Rests” instead of “Head Restraints”, and actually have them adjusted improperly (all the way down). The purpose of these devices is not to “rest” your head because you are tired, it is to “restrain” your head from flying backwards during a rear-ender accident. The top of the Head Restraint should be level with the top of your head, and the gap between the two should not be more than about two inches. For the record; if you recline your seat more than 20 degrees, all bets are off. A serious rear-ender will cause you to ramp up in your seat rendering the Head Restraint useless.
2018 Destroy Chronic Pain / Doctor Russell Schierling
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Whiplash Injuries Explained" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



