Degenerative Arthritis
- Spinal Arthritis:
- Spondylosis aka Degenerative disease of the spine represents an evolution of changes affecting most mobile spinal segments beginning with:
- Intervertebral disc (IVD) dehydration (desiccation) and degeneration aka Degenerative Disc Disease (DDD) with an abnormal increase in mechanical stress and degeneration of posterior elements affecting 4-mobile synovial articulations ( true osteoarthritis)
- 2-Facets in the L/S & 2-Facets & 2-Uncovertebral joints in the C/S
- Imaging plays a significant role in the diagnosis, grading, and evaluation of neurological complications (e.g., spondylotic myelopathy/radiculopathy)
- X-radiography with AP, Lateral & Oblique spinal views provides Dx and classification of Spondylosis
- MR imaging may help to evaluate the degree of neurological changes associated with degenerative spinal canal and neural foraminal stenosis
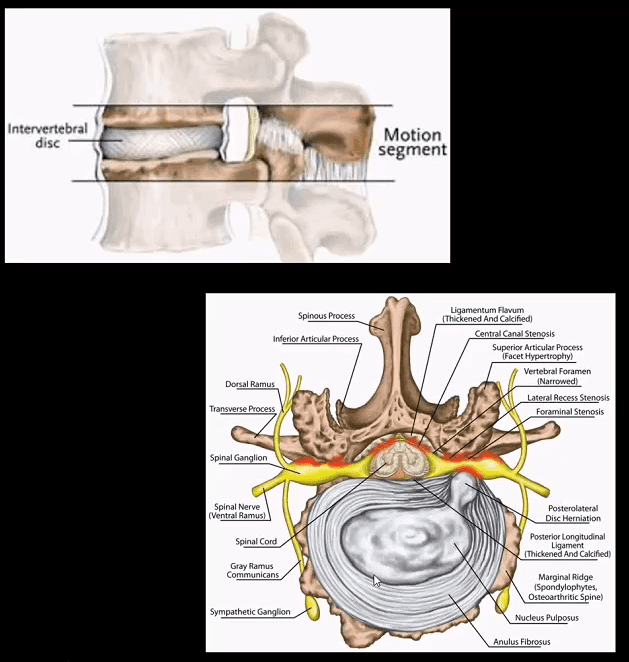
- Spinal motion segment:
- 2-adjacent vertebrae
- IVD (fibrocartilage)
- 2-facets (synovial)
- Pathology: loss of disc height increases mechanical stress on mobile elements
- Ligamentous laxity/local instability
- Spinal osteophytes aka spondylophytes & bony facet/uncinate proliferation
- Disc herniation and often disc-osteophyte complex
- Ligamentum flavum “hypertrophy” or thickening due to buckling
- Loss of normal lordosis with or w/o reversal or kyphosis
- Vertebral canal & neural foraminal stenosis
Neutral lateral cervical radiograph: note mild to moderate disc narrowing and spondylophyte formation at C5-6 & C6-C7 (most common levels affected by cervical spondylosis). Straightening or flattening with mild reversal of cervical lordosis. Some mild facet proliferation is noted at the above levels
- On radiographs: evaluate for disc height (mild, moderate or severe) loss
- End-plate sclerosis & spondylophytes; mild, moderate or severe
- Facet and uncinate irregularity, hypertrophy/degeneration; mild, moderate or severe
- Note degenerative instability aka degenerative spondylolisthesis/retrolisthesis
- Normal or lost lordosis vs. degenerative kyphosis
- Key Dx: correlate with a clinical presentation: neck/back pain with or w/o neurological disturbance ( myelopathy vs. radiculopathy or both)
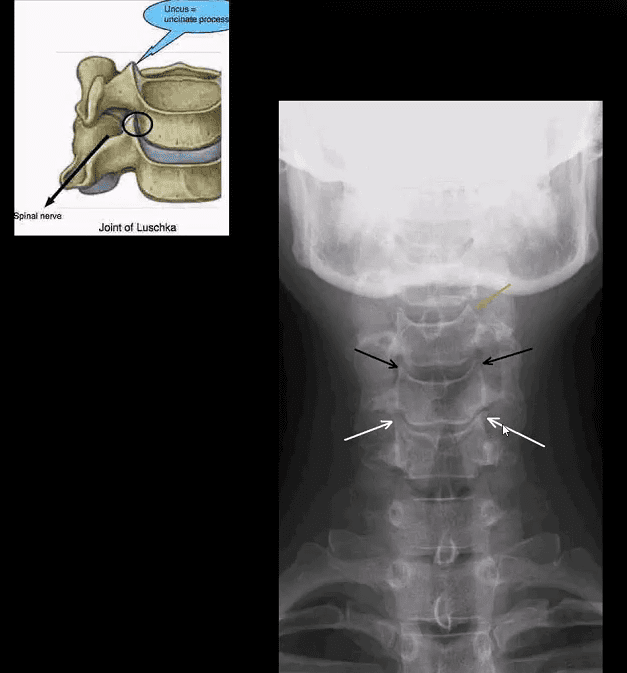
- Uncinate processes undergo degeneration/proliferation resulting in uncovertebral arthrosis
- Early findings present with mild bone proliferation along the cortical margin (white and black arrows) if compared to normal uncinate (orange arrow)
- Later, more extensive bone proliferation extending into and narrowing vertebral canal and neural osseous foramina (IVF’s) may be noted. The latter may contribute to spinal/IVF stenosis and potential neurological changes
- Posterior oblique views may help further
- AP lower cervical (a) and posterior oblique (b) views
- Note mild uncinated process proliferation with neural foraminal narrowing (arrows)
- Typically if less than a third of IVF becomes narrowed, patients may present w/o significant neurological signs
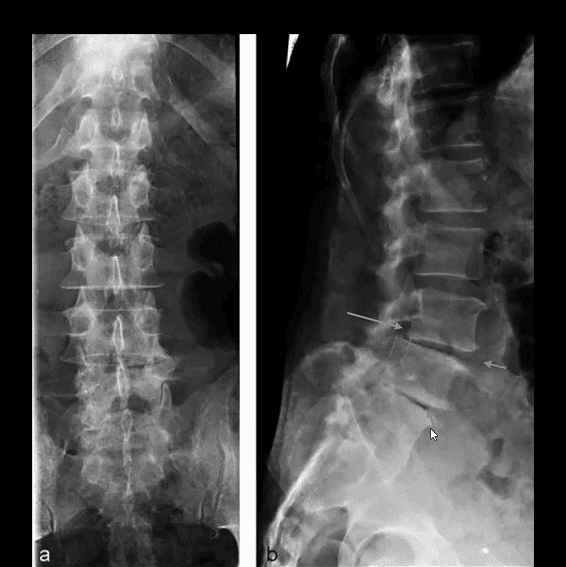
- Lumbar spondylosis is evaluated with AP and lateral views with additional AP L5-S1 spot view to examine lumbosacral junction
- Typical features include disc height loss/degeneration
- Intra-discal gas (vacuum) phenomenon (blue arrow) along with spondylophytes
- Degenerative spondylolisthesis and/or retrolisthesis (green arrow) may follow disc and facet degeneration and can be graded by the Meyerding classification
- In most cases, degenerative spondylolisthesis rarely progresses beyond Grade 2
- Lumbar facet degeneration seen as bone proliferation/sclerosis and IVF narrowing
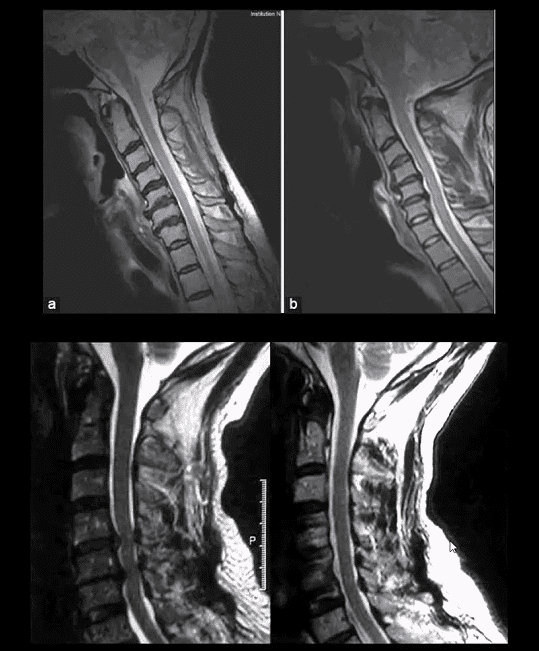
- MR imaging w/o gad C is an effective modality to evaluate clinical signs of spondylosis & associated neurological complications with pre-surgical evaluation
- Case: 50-y.o Fe with neck pain. Case b-45-y.o.M (top a b images). MRI reveals: loss of disc hydration or desiccation, spondylophytes and disc herniation w/o neurological changes
- (Bottom images) Left: preoperative and right postoperative MRI slices of the patient presented with clinical signs of cervical spondylotic myelopathy. Note disc herniation, ligam flavum hypertrophy and canal stenosis (left)
- Sagittal MRI slice of lumbar DDD manifested with disc desiccation and posterior herniation effacing thecal sac
- Correlating sagittal and axial slices will be more informative to evaluate canal stenosis and potential degree of neurological involvement (above-bottom images)
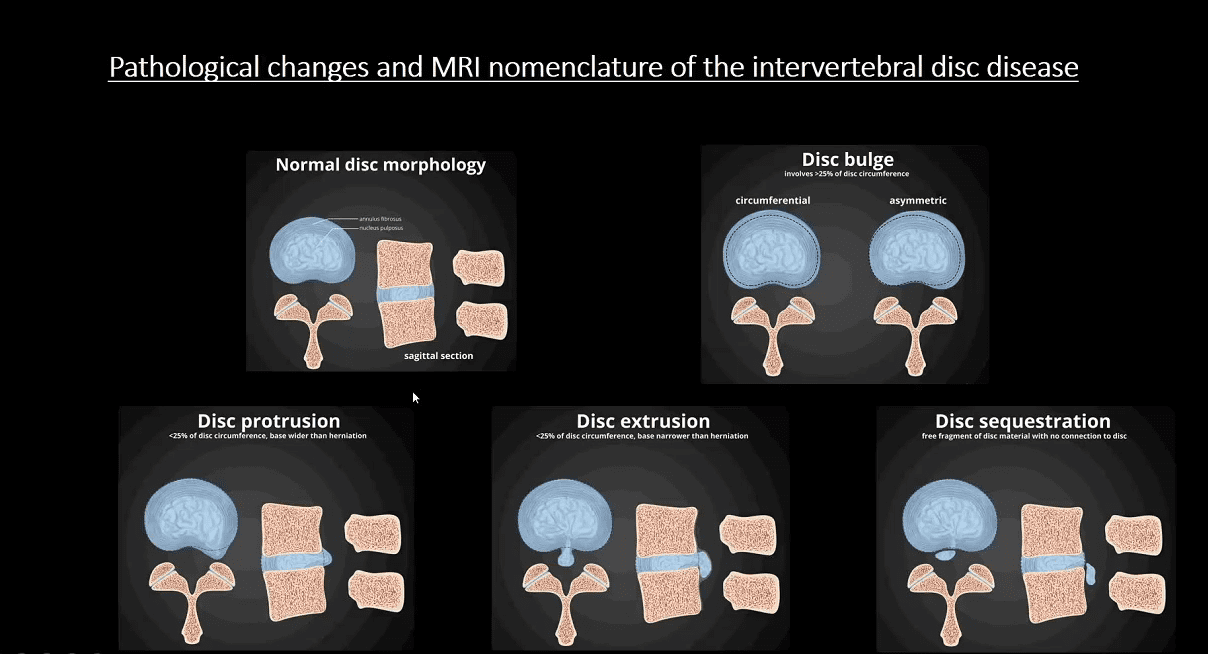
- Use the following resources to learn more on MRI evaluation and diagnosis of Degenerative Disc Disease:
- https://radiopaedia.org/articles/intervertebral-disc-disease-nomenclature
- https://ac.els-cdn.com/S1529943014004094/1-s2.0-S1529943014004094-main.pdf?_tid=bab686bc-cf70-4479-a243-b6d2b342461c&acdnat=1535573367_98364d2d06b7c967d3e859e785eb6f13
Diffuse Idiopathic Skeletal Hyperostosis (DISH) aka Forestier disease
- Flowing degenerative ossification of ALL
- M/c Thoracic spine. 2nd m/c-cervical spine
- Dx by imaging only. X-radiography is sufficient
- CT w/o contrast helps with Dx of Fx
- Men>women. Pts>60-y.o. Extensive DISH shows 49% association with type 2DM
- Complications: Chalk (carrot) stick Fx. Unstable 3-column Fx requiring surgical fusion
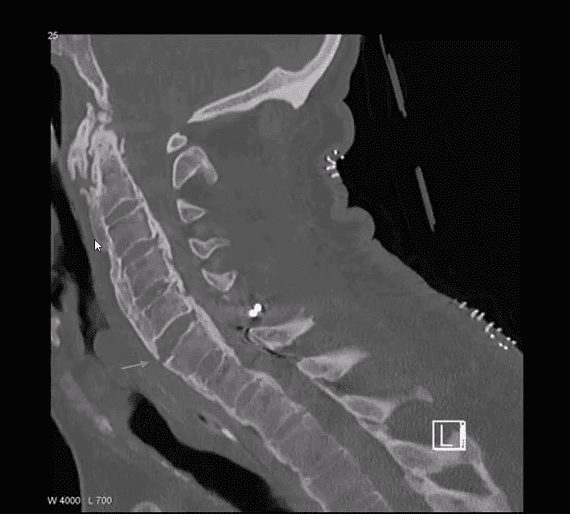
- Sagittal reconstructed CT scan slice in bone window
- Chalk stick Fx at C5-C6 in the patient with DISH and OPLL
Spinal Arthritis
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Spinal Arthritis Diagnostic Imaging Approach Part I" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



