- Spinal Arthritis
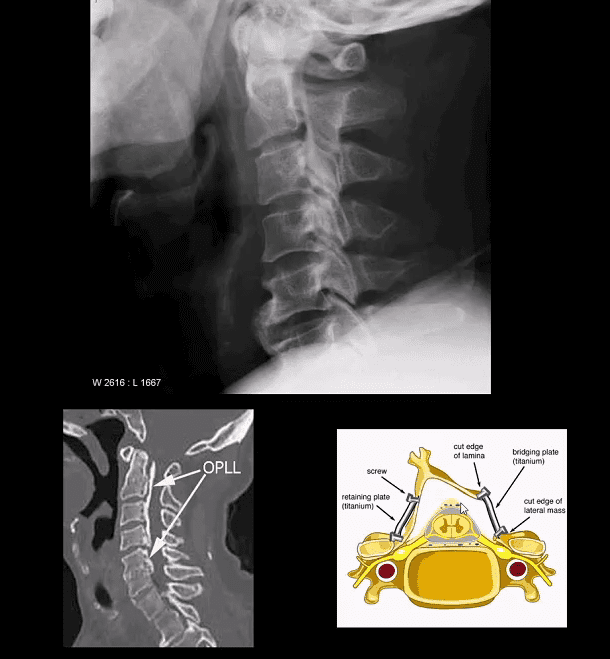
- Ossification of Posterior Longitudinal Ligament (OPLL). Less frequent than DISH.
- Greater clinical importance d/t spinal canal stenosis and cervical myelopathy
- Asian patients are at higher risk
- Both OPLL & DISH may co-exist and increase the risk of Fx
- Imaging: x-rad: linear radioopacity consistent with OPLL
- Imaging modality of choice: CT scanning w/o contrast
- MRI may help to evaluate myelopathy
- Care: surgical with laminoplasty (above right image) that has been pioneered and advanced in the Far East
M/C Inflammatory Arthritis In Spine
- Rheumatoid spondylitis (Rheumatoid arthritis) d/t inflammatory synovial proliferation pannus rich in lymphocytes, macrophages, and plasma cells
- C/S RA may affect 70-90% of patients
- Variable severity from mild to destructive disabling arthropathy
- RA IN C/S m/c affects C1-C2 due to an abundance of rich synovial tissue
- Typically infrequent in the thoracic/lumbar region
- Sub-axial C/spine may be affected later due to facets, erosions, ligament laxity and instability showing “Stepladder” appearance
- Clinically: HA, neck pain, myelopathy, etc. inc. Risk of Fx/subluxation. Any spinal manipulation HVLT ARE STRICTLY CONTRAINDICATED.
- Rx: DMARD, anti-TNF-alfa, operative for subluxations, etc.
Rheumatoid Spondylitis C1-C2. Perform X-radiography initially with flexed-extended views. Note Dens erosion, C1-2 subluxation (2.5 mm) that changes on mobility
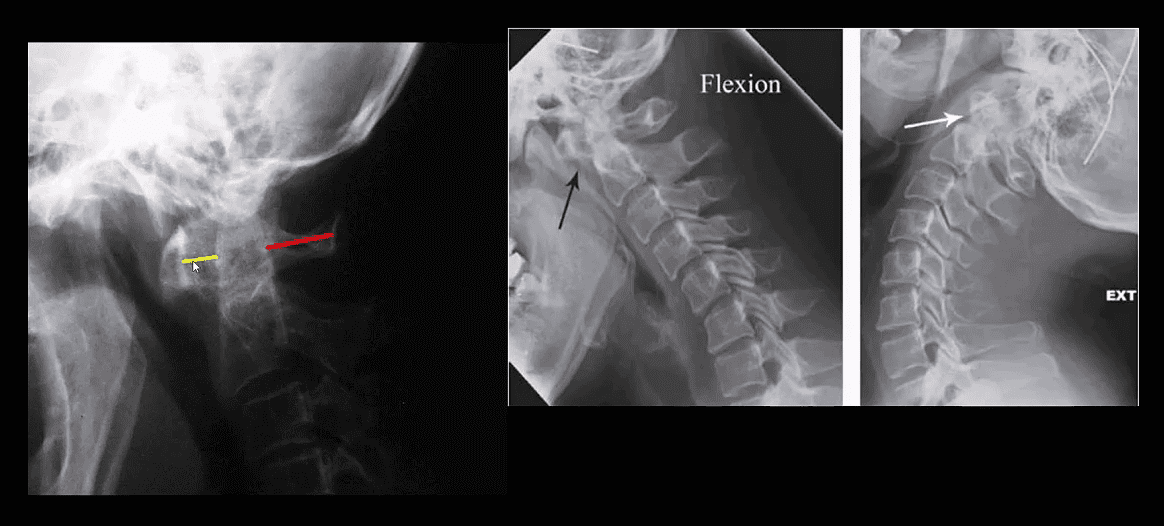
- RA spondylitis: an erosion of the odontoid with the destruction of C1-C2 ligaments and instability
- Stepladder aka Step-step sub-axial deformity d/t facets erosions and ligamentous destruction/laxity
- MRI required to evaluate cord compression/myelopathy
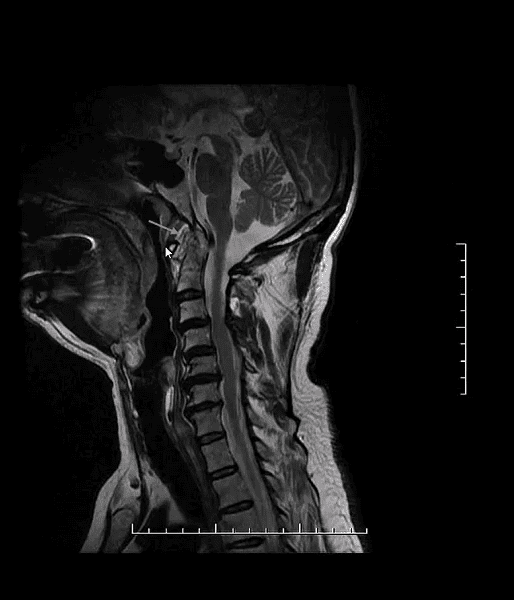
- Sagittal T2 WI MRI of pt with RA. Rheumatoid pannus formation is present at C1-2 (arrow) causing mild cord compression
- RA pannus may develop early before frank x-radiography changes noted
- Clinically: HA, neck pain, tingling in UE, positive Lhermitte phenomenon d/t cervical myelopathy
Operative Care of Rheumatoid Spondylitis and Its Complications
Seronegative Spondyloarthropathies
- Ankylosing Spondylitis (AS)
- Enteropathic Arthritis (EnA) (d/t IBD: Crohn’s & UC) identical to AS on imaging
- Psoriatic Arthritis (PsA)
- Reactive Arthritis (ReA)
- All share the following features: m/c HLA-B27 marker, RF-, Sacroiliitis, Enthesitis, Ocular Involvement (i.e., conjunctivitis, uveitis, episcleritis, etc.)
- AS & EnA are radiographically virtually indistinguishable, but EnA typically presents with less severe spinal changes than AS
- Both PsA & ReA present with virtually identical spinal changes, but ReA typically affects the lower extremity compared to PsA affecting hands and feet
- AS: likely autoimmune systemic inflammatory disease that targets SIJ, spinal facet joints annuls of the disc, rib joints and all spinal ligaments.
- Key path feature: enthesitis.
- Extraspinal features: uveitis, aortitis, pulmonary fibrosis, amyloidosis, cardiovascular disease.
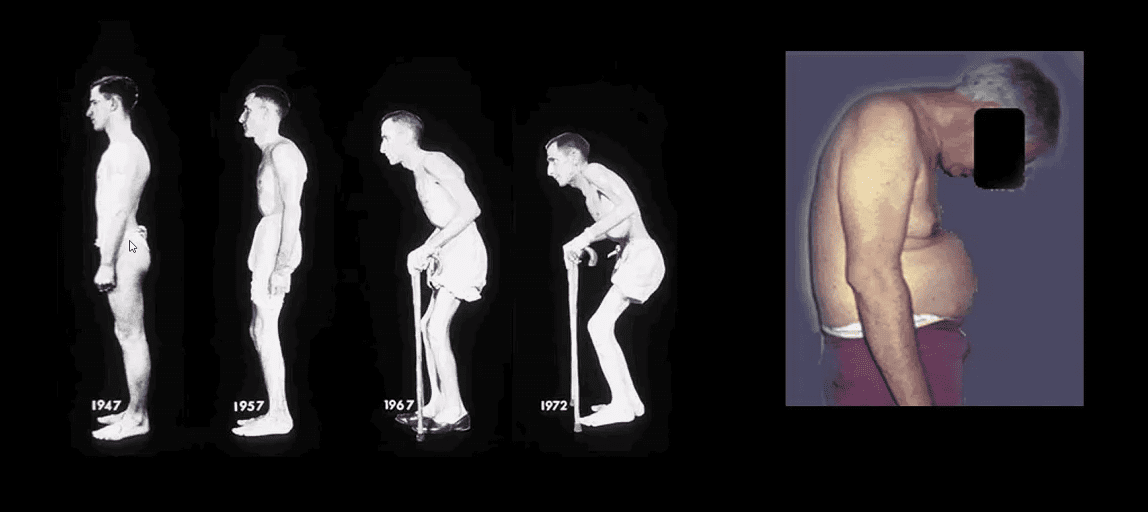
- M:F 4:1, age: 20-40 m/c. Clinic LBP/stiffness, reduced rib expansion <2 cm is > specific than HLA-B27, progressive kyphosis, risk of Fx’s.
- Imaging steps: 1st step-x-rays to id. Sacroiliitis/spondylitis. MRI & CT may help if x-rays are unrewarding.
- Labs: HLA-B27, CRP/ESR, RF-
- Dx: clinical+labs+imaging.
- Rx: NSAID, DMARD, anti-TNF factor therapy
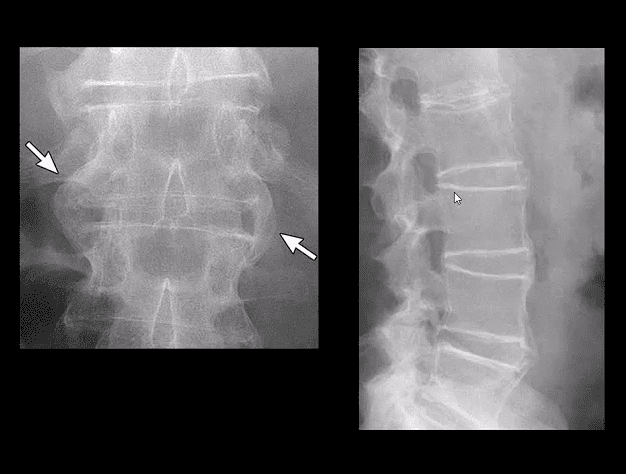
- Key Imaging Dx: always presents initially as b/l symmetrical sacroiliitis that will progress to complete ankylosis. Spondylitis presents with continuous ascending discovertebral osteitis (i.e., marginal syndesmophytes, Romanus lesion, Anderson lesion), facets and all spinal ligament inflammation and fusion with a late feature of “bamboo spine, trolley track, dagger sign,” all indicating complete spinal ossification/fusion. Increasing risk of Fx’s.
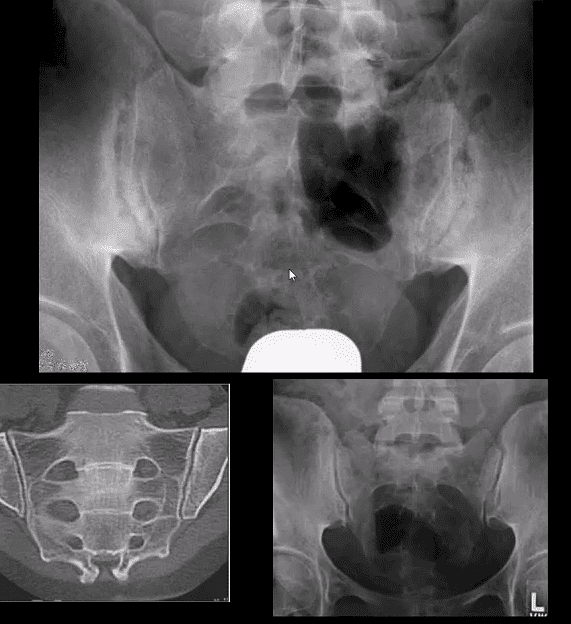
Key Dx of Sacroiliitis
- Blurring, cortical indistinctness/irregularity with adjacent reactive subchondral sclerosis initially identified primarily on the iliac side of SIJs.
- Normal SIJ should maintain a well defined white cortical line. Dimension 2-4 mm. May look incongruous d/t 3D anatomy masked by 2D x-rays.
Key Imaging Dx In Spine
- Marginal syndesmophytes and inflammation at the annulus-disc (above arrows) at the earliest dx; by MRI as marrow signal changes on T1 and fluid sensitive imaging (above top images).
- These represent enthesitis-inflammation that will ossify into bamboo spine.
- Lig ossification: trolley track/dagger sign
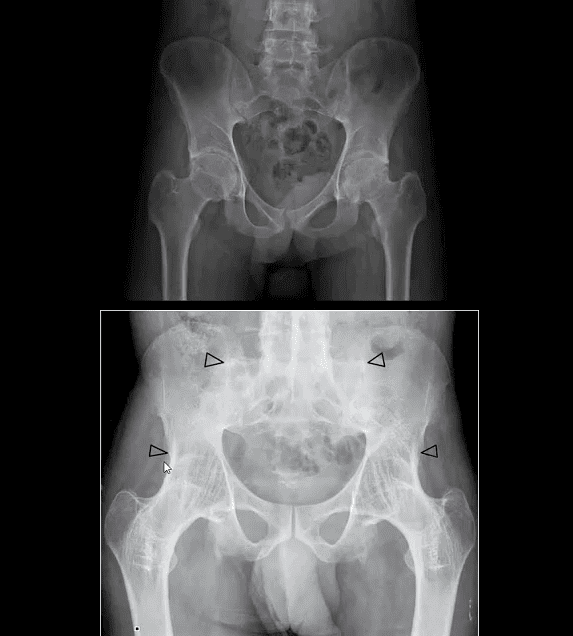
- AS in extraspinal joints: root joints, hips, and shoulders
- Symphysis pubis
- Less frequent in peripheral joints (hands/feet)
- All seronegatives may present with heel pain d/t enthesitis
- Complication: Above Carrot-stick/chaulk-stick Fx
- PsA & ReA (formerly Reiter’s) present with b/l sacroiliitis that virtually identical to AS
- In the spine PsA & ReA DDx from AS by the formation of non-marginal syndesmophytes aka bulky paravertebral ossifications (indicate vertebral enthesitis)
- For a clinical discussion of Spondyloarthropathies refer to:
- https://www.aafp.org/afp/2004/0615/p2853.html
Spinal Arthritis
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Spinal Arthritis Diagnostic Imaging Approach Part II" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



