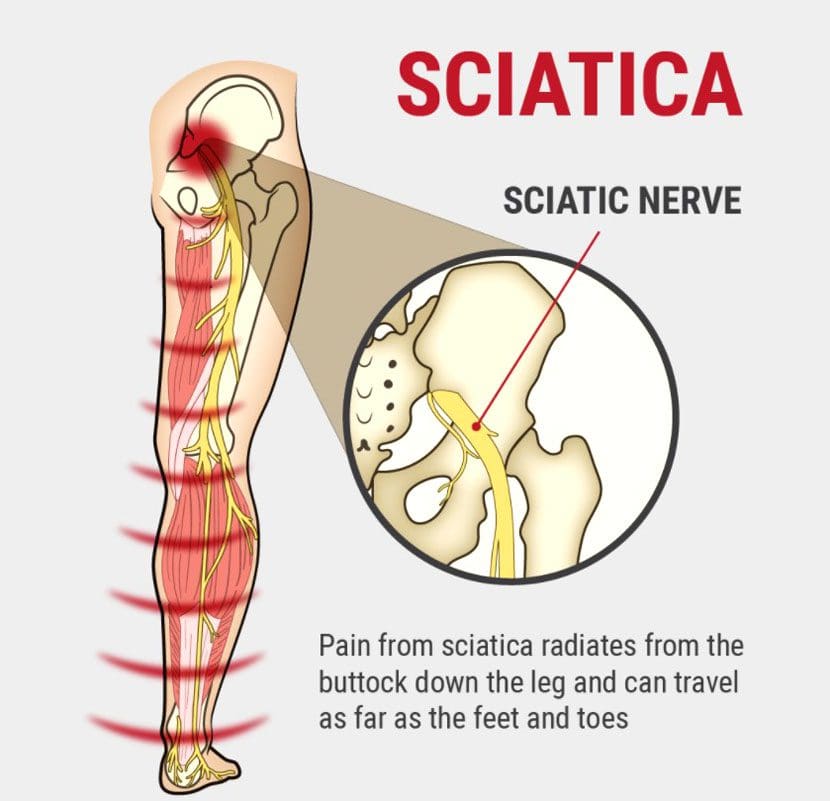
Sciatic nerve injury happens from trauma to the nerve and can cause numbness, tingling, loss of muscle power, and pain. The traumatic experience can be a muscle spasm that pulls and/or pinches the sciatic nerve, force/pressure impact injury, over-stretching injury, or a laceration/cutting injury. A slipped disk, or herniated disk, is the most common cause of irritation on the sciatic nerve. A slipped disk occurs when one becomes slightly dislodged, pushing out from the spine. This places pressure/compression on the sciatic nerve.
Sciatic Nerve Injury Causes
Trauma
- Hip dislocation
- Acetabular fracture
- Trauma to the lower back, buttocks, or leg from an automobile accident, sports injury, work injury.
Medical treatment causes:
- Direct surgical trauma.
- Total hip replacement surgery can cause nerve compression and stretch during the procedure, causing damage to the sciatic nerve resulting in dysfunction.
- Faulty positioning during anesthesia.
- Injection of neurotoxic substances.
- Injection injuries via intramuscular injection in the gluteal region. This is a situation where there is a loss of movement and or lack of sensation at the affected lower extremity with or without pain.
- Injection palsy can begin suddenly or hours following damage to the sciatic nerve.
- A misplaced intramuscular injection at the gluteal region is the most common cause of injury. It is attributed to frequent injections or poor techniques resulting from inadequately trained or unqualified staff.
- Tourniquet-Induced Sciatic Nerve Injury.
- Dressings that are too tight.
- Casts that impinge the nerve.
- Faulty fitting orthotics.
- Post radiation treatment can cause acute and delayed muscle damage.
Clinical Presentation Symptoms
The common symptoms are pain and abnormal walking gait. Other clinical symptoms include:
- Muscular weakness/atrophy
- Reflex impairment
- Motor and sensory issues like paraesthesia and numbness
- Foot drop
- External rotation of the hip
- Abduction contracture of the hip
- Equinus deformity
Medical History
- Complaints of radiating pain in the leg, which follows a sensory nerve pattern.
- Pain radiates below the knee, into the foot.
- Complaints of low back pain, which is often less severe than leg pain.
- Report of electrical, burning, numbing sensations.
Diagnosis
A detailed subjective and objective physical examination is necessary to figure out the severity of the sciatic nerve injury. Diagnostic studies include:
- X rays
- Electromyography
- Magnetic Resonance Imaging
Chiropractic and Physical Therapy Management
Conservative treatment is the first-line approach for managing a sciatic nerve injury.
Pain Management
- TENS
- Massage
- Gentle stretching
- Desensitization techniques
Exercise and Stretches
- Chiropractic and physical therapy exercises and stretches improve nerve regeneration after nerve damage.
Electrical Muscle Stimulation
- TENS and Electroacupuncture have been shown to help enhance nerve regrowth.
- Bio-laser stimulation can help with nerve nutrition and regeneration.
Joint or Soft Tissue mobilization
- Helps to retain muscle, nerve, and soft tissue flexibility and prevent deformity.
Balance Training
- Coordination, strength, and flexibility exercises help to restore balance.
Splinting
- In the early stages after a sciatic nerve injury, bracing may be needed to prevent deformity and new injury or re-injury risks.
- Ankle Foot Orthosis – AFO can help prevent foot drop, muscle damage, and falls risk.
Body Composition
Optimize Diet for Fat Loss
Individuals that want to lose fat need to create a calorie deficit. Individuals need to consistently eat less than they need for Total Daily Energy Expenditure – TDEE. The safest way to handle a caloric reduction is to reduce calorie intake in small doses like 200-300 calories, for example. After a week or two, perform a body composition analysis. If Fat Mass numbers begin to drop or not, adjust calorie needs accordingly. Restricting calories is the most common way, a deficit can also be created by increasing calorie needs through exercise.
References
Kline, D G et al. “Management and results of sciatic nerve injuries: a 24-year experience.†Journal of neurosurgery vol. 89,1 (1998): 13-23. doi:10.3171/jns.1998.89.1.0013
Schmalzried, TP et al. “Update on nerve palsy associated with total hip replacement.†Clinical Orthopedics and related research,344 (1997): 188-206.
Shim, Ho Yong et al. “Sciatic nerve injury caused by a stretching exercise in a trained dancer.†Annals of rehabilitation medicine vol. 37,6 (2013): 886-90. doi:10.5535/arm.2013.37.6.886
Suszyński, Krzysztof et al. “Physiotherapeutic techniques used in the management of patients with peripheral nerve injuries.†Neural regeneration research vol. 10,11 (2015): 1770-2. doi:10.4103/1673-5374.170299
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Sciatic Nerve Injury" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



