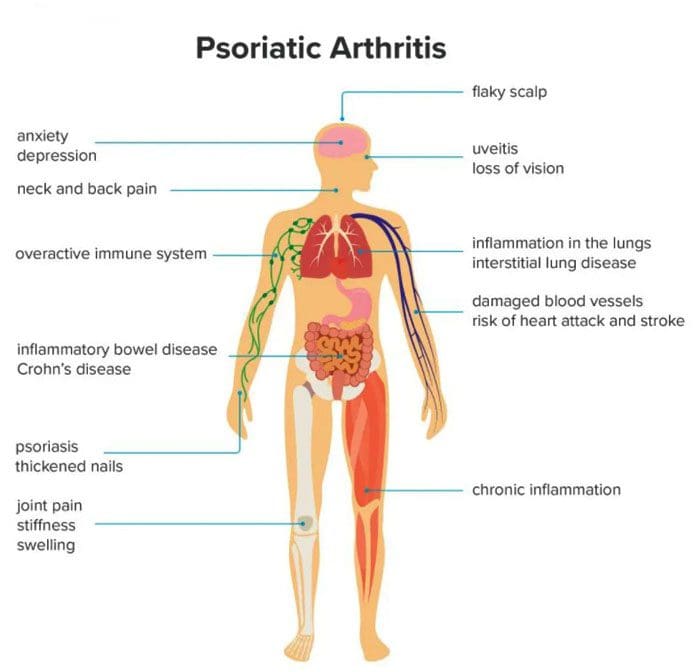
Psoriatic arthritis can develop in individuals who have psoriasis, affecting various joints, especially the knees. Psoriasis is a skin condition that causes skin cells to build up and form patches of itchy, dry skin known as plaques. Psoriatic arthritis is a long-term inflammatory disease that can cause inflammation, stiffness, and pain. Symptoms can progressively worsen over time without treatment. Early diagnosis is vital to minimize damage to the joints and slow the condition’s progress with treatment.
Psoriatic Arthritis
Psoriatic arthritis symptoms like stiffness and swelling can present differently from person to person. For example, some individuals with psoriatic knee arthritis will experience stiffness or pain in one knee, while others experience symptoms in both knees. Psoriatic arthritis in the knee can also cause swelling in the surrounding:
- Ligaments
- Tendons
- Synovial membranes
- Symptoms can also present in the:
- Elbows
- Feet
- Hands
Symptoms
Symptoms usually begin between the ages of 30 and 50. Common symptoms include:
- Stiffness after resting or sleeping.
- Swelling.
- Inflammation in the knee and surrounding area.
- Warm or hot skin on the knee from the inflammation.
- Pain in and around the joints, tendons, or ligaments.
- Joint sticking, difficulty moving, or reduced range of motion.
Other symptoms include:
- Back pain
- Fatigue
- Pain and redness in the eyes
- Swollen fingers or toes
- Difficulty walking from pain in the feet or Achilles tendon.
- Nail pitting or separation.
The severity of psoriasis does not determine psoriatic arthritis symptoms. Symptoms can go through a pattern of relapses and remissions. Individuals can have a sudden attack where symptoms get worse over a short time. After the flare-up, symptoms can improve as the condition goes into remission. Symptoms may not present for a long time until another flare-up. For example, an individual may have severe psoriasis but only mild psoriatic arthritis.
Causes
Psoriatic arthritis develops when the body’s immune system mistakenly attacks healthy cells and tissues. The faulty immune response causes the body to quickly generate new skin cells that stack on top of each other forming plaques. When the condition affects the joints, it leads to inflammation. While there is no apparent cause for psoriatic arthritis, researchers have found connections to genetics and the environment, as well as, individuals with close relatives that have psoriatic arthritis could be more likely to develop the condition. Other factors that could influence the development include:
- Severe psoriasis
- Traumatic injury/s
- Obesity
- Nail disease
- Smoking
The condition can happen at any age, but according to the National Psoriasis Foundation, most individuals first notice symptoms about ten years after their psoriasis begins. However, only 30% of individuals with psoriasis develop psoriatic arthritis.
Diagnosis
Doctors use imaging tools to diagnose psoriatic arthritis in the knee. They will use:
- MRI
- X-rays
- Ultrasound
- To help them check for irregularities or signs of inflammation in the joint and surrounding tissues.
- Additional tests are used to rule out other common forms of arthritis like rheumatoid and osteoarthritis.
- Blood tests check for inflammation and specific antibodies.
- In some cases, a small amount of fluid from the joint is taken to help eliminate the possibility of other underlying conditions like an infection.
Treatment
There is currently no cure for psoriatic arthritis, but treatments are being developed and show promise for long-term management. Current treatments focus on managing symptoms and improving the quality of life for the individual.
Biologics
Biologic medications like tumor necrosis factor or TNF inhibitors are recommended as the first-line therapy for most individuals with a new diagnosis of psoriatic arthritis. These meds help block TNF, which plays a crucial role in inflammation. They have shown to be effective at reducing the severity of symptoms and the frequency of flare-ups. Biologics can cause unwanted side effects, especially in individuals that experience frequent infections and need routine monitoring.
Small Molecule Medications
Individuals that cannot use biologic medications may be recommended a new class of medication called oral small molecules or OSMs. Examples include apremilast – Otezla and tofacitinib – Xeljanz.
Disease-modifying Antirheumatic Drugs
Disease-modifying antirheumatic drugs – DMARDs are a long-term option. They are used to slow the progression of psoriatic arthritis, and examples include methotrexate and cyclosporine. DMARDs work best when an individual begins taking them as early as they can take time to work. However, individuals are encouraged to continue taking them, even if symptoms do not improve right away.
Easing Inflammation
A doctor may prescribe nonsteroidal anti-inflammatory drugs – NSAIDs and corticosteroid injections when knee symptoms flare-up. These are short-term treatments that provide immediate relief, as long-term use can lead to side effects. Individuals can find relief with combined self-care that includes:
- Taking over-the-counter NSAIDs like ibuprofen/Advil or naproxen/Aleve.
- Applying ice and heat packs.
- Gentle exercise to promote a full range of motion.
- Gentle stretching or yoga can help relax tight muscles.
- Chiropractic.
- Acupuncture.
- Therapeutic Massage.
- Anti-inflammatory diet.
- Electrical stimulation.
Chiropractic treatment can help to:
- Relieve soreness.
- Prevent muscle spasms.
- Realign joints.
- Improve mobility.
However, chiropractic is not the primary treatment for arthritis but is intended to be used in combination to relieve pain, loosen and stretch the muscles and balance the body.
InBody
Strength, Balance, and Improved Body Composition
Functional fitness is the ability to move comfortably every day. The benefits of physical activity also contribute to improved body composition. Working to reach a certain level of functional fitness can help the aging process that has been shown to reduce metabolic rate. Inactivity is why individuals lose Lean Body Mass as they age, leading to increased body fat. Lean Body Mass contributes to the body’s overall Basal Metabolic Rate or BMR, also known as metabolism. This is the number of calories the body needs to support essential functions. Everyone is encouraged to engage in strength training or resistance exercises, but specifically older adults. This can help regain muscle loss which can lead to an increase in lean body mass. The increase in Lean Body Mass increases BMR, which helps prevent fat gain.
References
Chang, K. L., et al. (2015). Chronic pain management: Nonpharmacological therapies for chronic pain [Abstract]. https://www.ncbi.nlm.nih.gov/pubmed/25970869
Chiropractic care for arthritis. (n.d.). arthritis.org/health-wellness/treatment/complementary-therapies/physical-therapies/chiropractic-care-for-arthritis
Chiropractic: In-depth. (2019). nccih.nih.gov/health/chiropractic-in-depth
How to achieve remission in psoriatic arthritis. (n.d.). arthritis.org/diseases/more-about/how-to-achieve-remission-in-psoriatic-arthritis
Living with psoriatic arthritis. (n.d.). psoriasis.org/living-with-psoriatic-arthritis/
Sankowski, A. J., et al. (2013). Psoriatic arthritis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3596149/
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Psoriatic Arthritis Knee Pain" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



