- This is a brief review of some of the essential pediatric complaints encountered in clinical practice.
- Acute Trauma including acute head trauma
- Non-accidental Trauma in children (battered child)
- Musculoskeletal Complaints (Juvenile Idiopathic Arthritis, scoliosis,
- Common pediatric neoplasms (CNS & others)
- Infection
- Metabolic disease
Acute Pediatric trauma:

- FOOSH injuries (e.g. fell off the monkey-bar)
- Supracondylar Fx, elbow. Always d/t accidental trauma. <10-y.o.
- Extra-articular Fx
- Gartland classification grades minimally displaced subtle injuries treated with simple immobilization vs. posterior elbow dislocation treated operatively
- A potential risk of ischemic compromise if care is delayed (Volkmann contracture)
- The Radiological exam is crucial: sail sign & posterior fat pad sign with anterior humeral line failed to intersect mid/2/3 of Capitellum.
Incomplete pediatric Fx:
- most in <10 y.o. Greenstick, Torus, Plastic aka Bowing deformity
- Typically heal well, treated conservatively with immobilization
- Plastic deformity if >20-degrees requires closed reduction
- Ping pong skull fracture may develop following trauma, forceps delivery and complications of birth trauma. May need to be assessed by the pediatric neurosurgeon
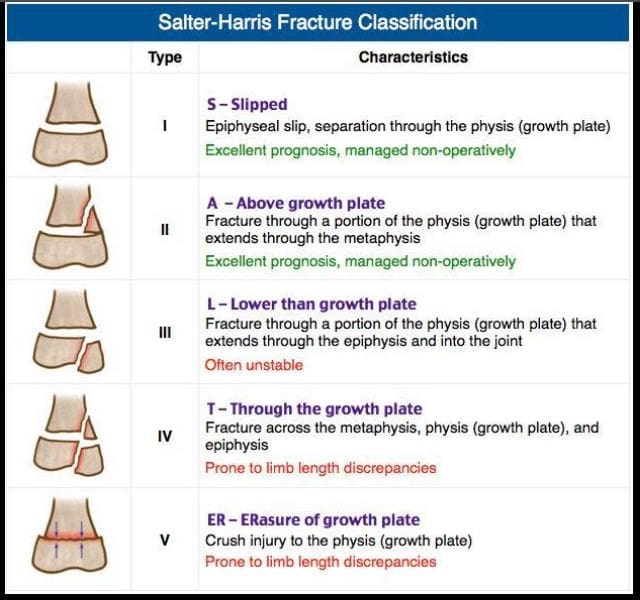
- Salter-Harris types of physeal growth plate injuries
- Type 1-slip. e.g., Slipped Capital Femoral Epiphysis. Typically no bone fracture noted
- Type 2-M/C with good prognosis
- Type 3- intra-articular, thus carries the risk of premature osteoarthritis and may require operative care d/t being unstable
- Type 4- Fx through all regions about the physis. Unfavorable prognosis and limb shortening
- Type 5- often no evidence of actual bone fracture. Poor prognosis d/t crush injury and vascular damage with limb shortening
- Imaging evaluation is crucial
Non-Accidental Injury (NAI)in Children
- There different forms of child abuse. Physical abuse may range from skin injuries to different MSK/systemic injuries affecting bones and soft tissues. Imaging is crucial and may identify definite signs alerting medical providers and informing child protection services and law enforcement agencies about physical abuse.
- In an infant: “shaken baby syndrome” may present with CNS signs d/t tearing of immature bridging vein and subdural hematoma which can be fatal. Retinal hemorrhaging often a clue. Head CT is crucial.
- MSK Radiological Red Flags:
- 1) major bone Fx in an un-ambulatory very young child (0-12 m.o.)
- 2) Posterior ribs Fx: naturally never occur d/t accidents. Most likely mechanisms: grabbing and squeezing a child or direct hit.
- 3) Multiple Fractures with different chronological healing rates, i.e., bone calluses indicating repeated physical trauma
- 4) Metaphyseal corner Fx aka Bucket handle Fx, often pathognomonic for NAI in children. Occurs when the affected extremity is held and violently twisted.
- 5) Spiral fracture of long bones in a young child is another example of NAI.
- Other important clues of NAI. Inconsistent history provided by guardians/caregivers. No evidence of congenital/metabolic bone abnormalities like Osteogenesis Imperfecta or Rickets/osteomalacia etc.
- N.B. When child’s guardians state a history that reports fall and accidents in the house, It is important to know that apparently most accidents/falls in the house are very rarely or unlikely result in major bone fractures.
- Reporting child abuse in Illinois:
- https://www2.illinois.gov/dcfs/safekids/reporting/pages/index.aspx
MSK Imaging Approach in Pediatrics
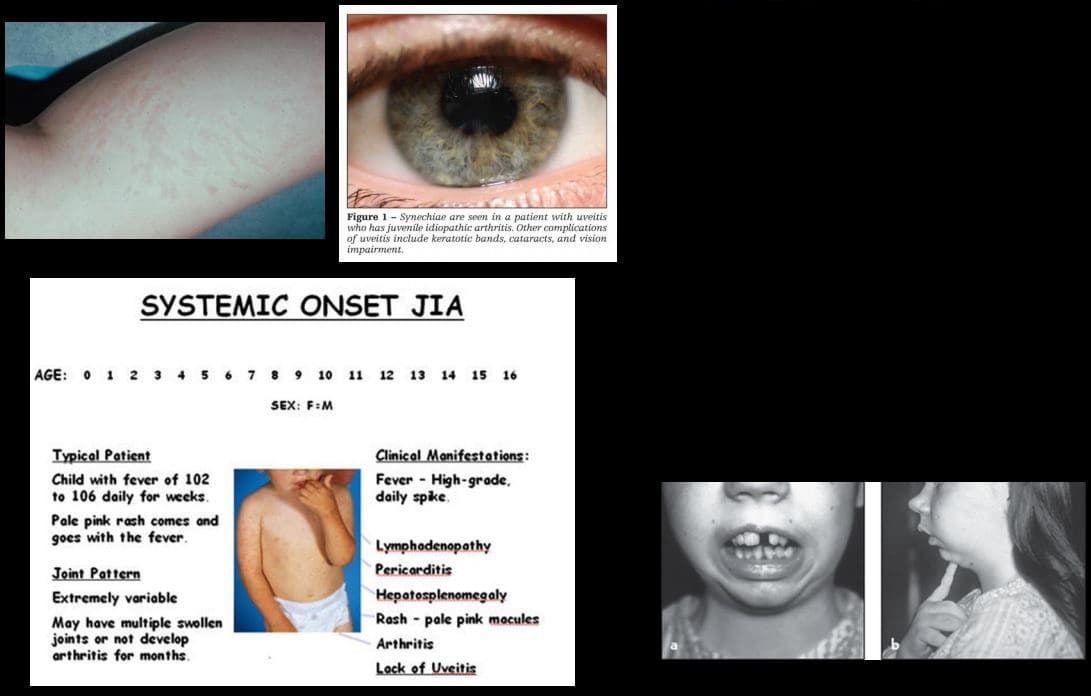
- Juvenile Idiopathic Arthritis (JIA)-considered M/C chronic disease of childhood. Clinical Dx: joint pain/swelling for 6-weeks or longer in a child <16-y.o. Different forms exist: Early Dx is crucial to prevent delayed complications
- Most familiar forms of JIA:
- 1) Pauciarticular disease (40%)- m/c form of JIA. Girls are at greater risk. Presents as arthritis in <4 joints: knees, ankles, wrist. Elbow. This type shows high association with ocular involvement as iridocyclitis (25%) that may potentially lead to blindness. Labs: RF-ve, ANA positive.
- 2) Polyarticular disease (25%): RF-ve. Girls are at greater risk. Affects small and large joints often affect Cervical spine
- 3) Systemic form of JIA (20%): often presents with acute systemic manifestation as spiking fevers, arthralgias, myalgias, lymphadeno[pathy, hepatosplenomegaly, polyserositis (pericardial/pleural effusion). Important Dx features characteristic evanescent salmon pink rash on the extremities and trunk. The Systemic form has a distinct lack of ocular involvement. Joints typically shoe no erosions compared to other types. Thus joint destruction is not typically seen
Imaging in JIA
- Joint effusion bone overgrowth squaring of patella cartilage/bone erosion superimposed DJD
- Fingers and long bones early physeal closure/limb shortening
- Rad DDx knee/ankle: Hemophilic arthropathy Rx: DMARD.
- Complications may occur joint destruction, growth retardation/limb shortening, blindness, systemic complications, disability.
Most Common Pediatric Malignant Bone Neoplasms
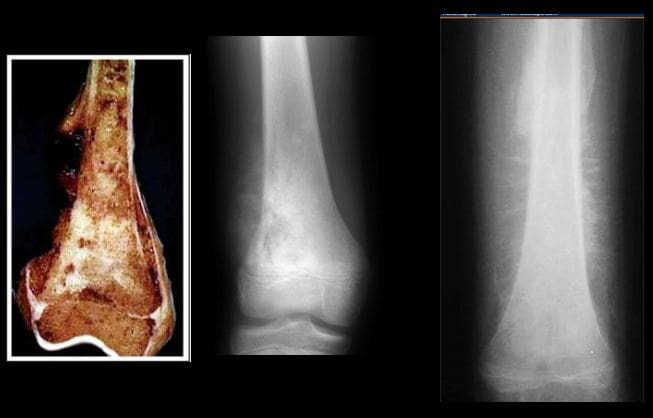
- Osteosarcoma (OSA) & Ewing’s sarcoma (ES) are 1 st and 2nd M/C primary malignant bone neoplasms of childhood (peak at 10-20 y.o.) Clinically: bone pain, change in activity, early metastasis especially pulmonary mets may occur. Poor prognosis
- Ewing’s may present with bone pain, fever and elevated ESR/CRP mimicking infection. Early Dx with imaging and staging are crucial.
- Imaging of OSA & ES: x-ray, followed by MRI, chest CT, PET/CT. On x-rays: OSA may affect any bone but most present as aggressive bone forming neoplasms about the knee (50% cases) especially as osteoid forming an aggressive lesion in the metaphysis with speculated/sunburst periostitis & Codman triangle. Marked soft tissue invasion.
- ES may present in the shaft and show very early soft tissue spread. MRI is crucial to reveal the extent of bone and ST invasion, MRI required for surgical planning
- OSA & ES Rx: A combination of surgery, radiation, chemo. Limb salvage techniques are performed in some cases. Poor prognosis if detected late.
- Imaging of Ewing’s sarcoma
- Permeating bone distraction
- Early and extensive soft tissue invasion
- Aggressive periosteal reaction with laminated (onion skin) response
- Saucerisation of cortical bone (orange arrow)
- A Lesion is typically diaphyseal with some metaphyseal extension
- Known as Round cell tumor along with Multiple Myeloma and Lymphoma
Common Childhood Malignancies
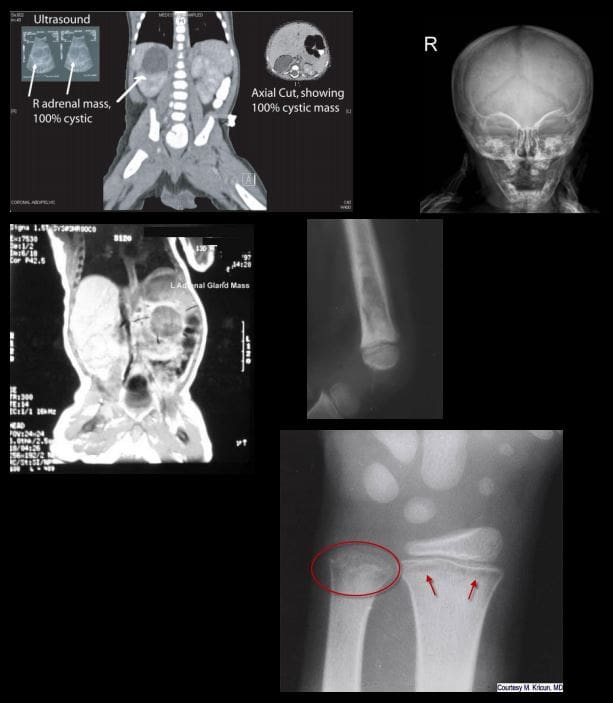
- Neuroblastoma (NBL) M/C malignancy of infancy. Derives from neural crest cells aka PNET tumors (e.g. sympathetic ganglia). Most occur in children <24-months. Some show good prognosis but >50% cases present with advanced disease. 70-80% at age 18-months or older present with advanced metastasis. NBL may develop in the adrenal medulla, sympathetic ganglia and other location. Presents as an abdominal mass, vomiting. >50% presents with bone pain d/t metastasis. Clinically: physical exam, labs, imaging: chest and abd x-rays, CT abdomen and chest is crucial to Dx. MRI may help. NBL may metastasize to the skull and infiltrate sutures with a
characteristic presentation as pathological sutural diastasis. - Acute Lymphoblastic Leukemia is the m/c malignancy of childhood. Pathology: leukemic cell infiltration of bone marrow leading to bone pain and replacement of other normal marrow cells with anemia, thrombocytopenia, neutropenia and associated complications. Leukemic cells may infiltrate other sites including CNS, spleen, bone and other regions. Dx: CBC, serum lactate dehydrogenase levels, Bone marrow aspiration biopsy is the key. Imaging may help but not essential to diagnosis. On radiography, leukemic infiltration of the bone may typically appear as radiolucent bands along the physeal growth plate. Rx: chemotherapy and treating complications
- Medulloblastoma: M/C malignant CNS neoplasm in children
- Majority develop before 10-y.o.
- M/C location: cerebellum and posterior fossa
- Histologically represents a PNET type tumor not a glioma as was originally thought
- MBL, as well as Ependymoma and CNS lymphoma, may lead to drop metastasis via CSF and additionally represent a unique that unlike other CNS tumors demonstrate metastatic spread outside CNS, m/c to the bone
- 50% of MBL may be fully resectable
- If Dx and treatment begin before metastasis, 5- year survival is 80%
- Imaging is crucial: CT scanning may be used but the imaging modality of choice is MRI that will additionally provide a
more superior evaluation of the entire neuraxis for metastasis. - MBL typically appears as heterogenous hypo, iso and hyperintense lesion on T1, T2 and FLAIR scans (top images) if compare to surrounding brain tissue. Often compressing 4th ventricle with obstructive hydrocephalus. The tumor typically shows contrast enhancement on T1+C gad (bottom left image). Drop metastasis from MBL with T1+C enhancing lesion in the cord
Important Pediatric Infections
- In the neonate/infant <1month: fever >100.4 (38C) may indicate bacterial and some viral infection. Strep B, Listeria, E. Coli may lead to sepsis, meningitis. Approach: chest x-ray, lumbar puncture with culture, blood culture, CBC, urinalysis.
- In young children, Hemophilus influenza type B (HIB) may lead to Epiglottitis a rare but serious complication. The current vaccine helps to reduce the number of cases of Epiglottitis and other HIB related illnesses.
- Parainfluenza or RSV virus may lead to Croup or acute Laryngotracheobronchitis.
- Epiglottitis and Croup are Dx clinically but AP and lateral soft tissue neck x-rays are very helpful
- Epiglottitis presents with a characteristic “thumb sign” that is consistent with thickened epiglottis d/t epiglottic edema. This can be a life-threatening emergency compromising airways (top left)
- Croup may show a “steeple sign” or “wine bottle sign” with distended hypopharynx as acute narrowing of subglottic airway on AP and lateral neck soft tissue x-ray (top right)
- Respiratory Syncytia Virus (RSV) and influenza may lead to viral pneumonia potentially with life-threatening complications in the immunocompromised, very young and children with comorbidities. CXR is crucial (middle left)
- Streptococcal pharyngitis with GABHS infection may lead to some acute or delayed complications (e.g. Rheumatic fever)
- Peritonsillar abscess (above middle right) may develop in some cases and be complicated by spreading along soft tissue planes in the neck potentially leading to spread into sublingual/submandibular spaces (Ludwig Angina) when airways need to be controlled d/t base of tongue edema
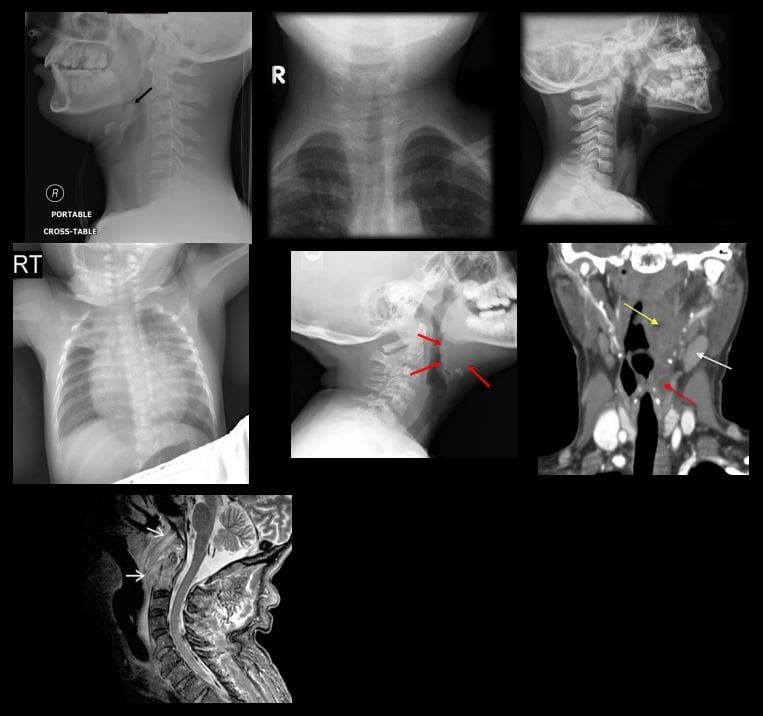
- Development of a retropharyngeal abscess may potentially lead to spread of the infection through freely communicating neck fascia resulting in necrotizing mediastinitis, Lemmier syndrome and invasion of carotid spaces (all are potentially life-threatening complications)
- Griesel syndrome- (above bottom left) rare complication of regional tonsillar/pharyngeal oral infections that can spread to prevertebral space leading to C1-2 ligaments laxity and instability
- Other important infections in children are typical bacterial (Pneumococcal) pneumonia, Urinary tract infection and Acute Pyelonephritis (especially in girls) and Meningococcal Meningitis
- Pediatric Metabolic Disease
- Rickets: considered osteomalacia in skeletally immature. Zone of provisional calcification of the epiphyseal growth plate is particularly affected
- Clinically presents with growth retardation, extremity bowing, rachitic rosary, pigeon chest, depressed ribs, enlarged and swollen wrists, and ankles, skull deformity
- Pathology: Vit D and calcium abnormality is the m/c cause. Lack of sun exposure esp. dark-skinned individual, restrictive clothing to light exposure, prolonged exclusive breastfeeding, veganism, malabsorption syndromes of the gut, renal damage and others
- Imaging: frayed metaphysis aka paint brush metaphysis with flaring, widening of the growth plate, bulbous costochondral junction as a rachitic rosary, extremity bowing
- Rx: treat underlying causes, correct nutritional deficit, etc.
References
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Pediatric Complaints Diagnostic Imaging Approaches | El Paso, TX." is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



