Mobility & Flexibility After Head Injuries: How Chiropractic & Integrative Care Help You Move Again

Key takeaway
Head injuries (also called traumatic brain injuries, or TBIs) can make movement slow and unsteady. You may experience muscle fatigue, poor coordination, and balance issues that affect walking, arm and leg movement, and overall stability. When you move less, stiffness and spasms can build up, leading to contractures and reduced flexibility. A well-planned program that blends chiropractic care (gentle spinal adjustments and joint mobilization), soft-tissue therapy, and targeted exercises can improve posture, circulation, nervous-system signaling, and day-to-day function while your brain adapts and heals (neuroplasticity). This article explains what’s happening in the body and outlines a simple, safe plan you can start discussing with your care team. (Headway, n.d.; MSKTC, 2018; BIAA, n.d.; Brain Injury Canada, n.d.) braininjurycanada.ca+3headway.org.uk+3MSKTC+3
How head injuries disrupt movement
1) Slower, less coordinated motion
After a head injury, mobility often becomes “slower,” with reduced balance and higher fall risk, especially when you’re fatigued or in pain. These changes can make walking harder, turning in bed slower, or getting dressed more difficult. Assistive devices may be needed in the short term or long term while you rebuild strength and control. (Headway, n.d.; Brain Injury Association of America, n.d.) headway.org.uk+1
2) Balance and gait changes can be subtle—but meaningful
Even “slight” changes in walking and balance can be functionally important. You may feel okay in a quiet room, but feel wobbly on uneven ground or when carrying groceries. These small deficits still matter for safety and independence and deserve evaluation and treatment. (BIAA, n.d.) Brain Injury Association of America
3) Fatigue makes symptoms worse
Fatigue after a TBI is common and can persist for an extended period, often exacerbating coordination and balance issues by the end of the day. That’s why pacing and rest breaks are part of good rehab plans. (MSKTC, 2018) MSKTC
4) Pain and neck involvement
Many people develop chronic pain after TBI, often including headaches and neck pain—sometimes tied to concurrent whiplash. Cervicogenic headaches (headaches referred from the neck) are frequent after concussive and acceleration-deceleration injuries. (Clinical Pain Advisor, 2017; AAPM&R KnowledgeNow, n.d.; Defrin et al., 2014) clinicalpainadvisor.com+2PM&R KnowledgeNow+2
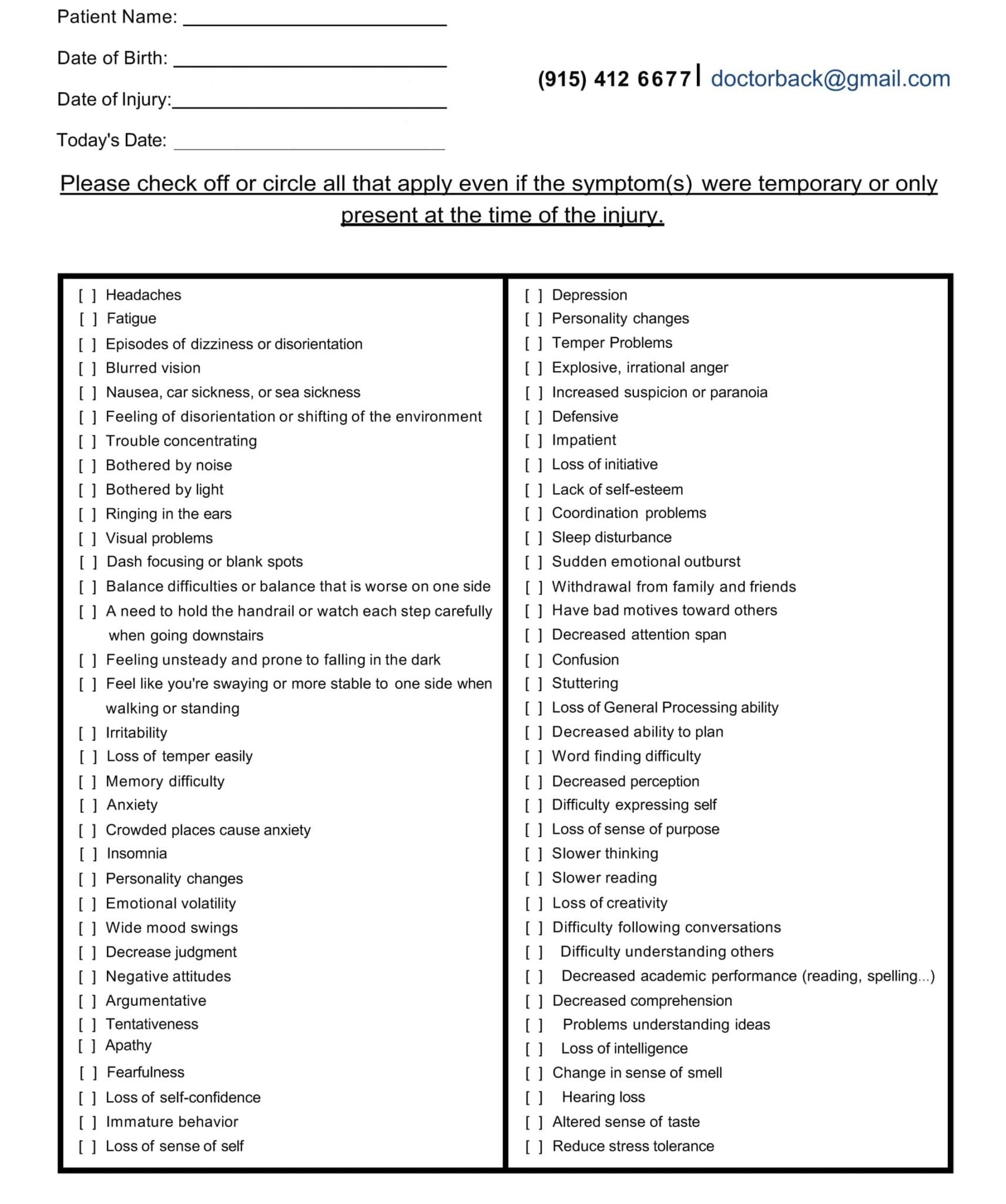
Symptom Questionnaire:
Why immobility leads to stiffness and contractures
When injuries limit movement, muscles tighten and joints stiffen. Over time, this can progress to contractures (permanent shortening of muscles or tendons), limiting range of motion and making hygiene, transfers, and gait training harder. Contributors include weakness, altered tone, and reduced activity—all common after head injuries. Early management, including stretching, positioning, splinting as needed, and graded mobility, helps prevent this cascade. (Physiopedia, n.d.; Neuro Rehab Times, 2024) Physiopedia+1
Movement disorders and hypokinesia after brain injury
Beyond weakness and balance loss, some people experience movement disorders such as tremor, dystonia, or myoclonus, and a general reduction in movement called hypokinesia. These problems, though less common than fatigue or dizziness, still impact flexibility and daily function and should be recognized and treated by a multidisciplinary team. (Moon et al., 2022) PMC
What a whole-person plan looks like
A strong recovery plan blends medical evaluation, therapeutic exercise, and hands-on care to restore range of motion and improve nervous-system control.
Physical therapy goals you should expect
-
Restore basic mobility (bed mobility, transfers, walking).
-
Re-train normal movement patterns and reduce abnormal compensations.
-
Improve endurance, balance, and safety for daily activities. (BIAA, n.d.) Brain Injury Association of America
Why chiropractic and integrative care help
In Dr. Alexander Jimenez’s dual-scope practice (Doctor of Chiropractic and Advanced Practice Registered Nurse), patients with head injuries often present with neck stiffness, posture changes, and limited joint glide in the cervical and upper thoracic spine. Gentle adjustments, mobilization, soft-tissue therapy, postural retraining, and vestibular-ocular drills help reduce cervicogenic headaches and improve balance, allowing patients to participate more fully in physical therapy. (DrAlexJimenez.com, 2025; 2025; 2023) El Paso, TX Doctor Of Chiropractic+2El Paso, TX Doctor Of Chiropractic+2
How it works (in simple terms):
-
Spinal adjustments and joint mobilization can restore segmental motion, reduce protective muscle guarding, and improve afferent (sensory) input to the nervous system. That improved input may support better balance strategies and posture control. (DrAlexJimenez.com, 2025; Impact Medical Group, 2024; Pinnacle Health Chiro, n.d.) El Paso, TX Doctor Of Chiropractic+2Impact Medical Group+2
-
Soft-tissue therapy (myofascial release, trigger point methods, instrument-assisted work) helps ease spasms and improve tissue slide, which supports flexibility and reduces pain during exercise. (DrAlexJimenez.com, 2025) El Paso, TX Doctor Of Chiropractic
-
Targeted exercises—including cervical stabilization, balance/vestibular drills, and dual-task training—speed up neuromotor relearning. (Cognitive FX, n.d.; DrAlexJimenez.com, 2025) CognitiveFX USA+1
-
Postural coaching (ergonomics, breathing mechanics, gait cues) reduces strain and helps your body use more efficient movement patterns. (DrAlexJimenez.com, 2025) El Paso, TX Doctor Of Chiropractic
Bottom line: These steps improve blood flow and cerebrospinal fluid dynamics locally, reduce nociceptive (pain) input from irritated joints and soft tissues, and support brain adaptation (neuroplasticity), allowing function to return. (DrAlexJimenez.com, 2025; Impact Medical Group, 2024) El Paso, TX Doctor Of Chiropractic+1
A step-by-step plan you can discuss with your care team
Always get medically cleared for exercise after a head injury and watch for red flags (worsening severe headache, vomiting, new neurologic deficits, confusion, neck instability, or vision changes). If any appear, stop and seek urgent care.
Phase 1: Calm the system and restore gentle motion (Days 1–14 after clearance)
-
Breathing reset (2–3 min, 3–5×/day): Slow nasal breaths with relaxed shoulders to reduce sympathetic overdrive and head/neck tension.
-
Cervical isometrics (pain-free): Gently press your head into your hand forward/back/side for 5 seconds, 5–8 reps.
-
Scapular setting: Light retraction/depression holds (5–10 seconds, 10 reps).
-
Ankle pumps and heel slides: Keep the legs moving to limit stiffness and support circulation.
-
Positioning for flexibility: Use a rolled towel under the neck (in a neutral curve) for 3–5 minutes, 1–2 times a day, and perform gentle chest/hip flexor stretches.
-
Chiropractic visit: Gentle cervical/thoracic mobilization or adjustment as appropriate, plus myofascial work for suboccipitals, scalenes, upper trapezius, and pectorals. (BIAA; Cognitive FX; DrAlexJimenez.com) Brain Injury Association of America+2CognitiveFX USA+2
Why this phase matters: It reduces muscle guarding, begins to restore joint play, and prepares you for balance and strength work without flaring symptoms. (MSKTC, 2018; Headway, n.d.) MSKTC+1
Phase 2: Balance, posture, and gait foundation (Weeks 2–6)
-
Vestibular-ocular drills (under supervision at first): smooth pursuits and gaze-stabilization (VOR) within comfort; progress from seated to standing.
-
Static balance to dynamic balance:
-
Feet together → semi-tandem → tandem stance (eyes open first), 20–30 seconds each.
-
Progress to head turns, then soft-surface standing.
-
-
Short, frequent walks: Start with 5–10 minutes, keeping symptoms below a 3/10 and using the “talk test” pacing method; add 1–2 minutes every other day.
-
Strength basics: Sit-to-stand, wall rows or band rows, mini-squats (2–3 sets of 8–12 reps).
-
Posture corrections: Chin nods, rib stacking, “stand tall—shoulders soft” every hour.
-
Chiropractic and soft-tissue care: Continue as needed to maintain cervical/thoracic motion, ensuring exercises remain comfortable and effective. (BIAA; MSKTC; Cognitive FX; DrAlexJimenez.com) El Paso, TX Doctor Of Chiropractic+3Brain Injury Association of America+3MSKTC+3
Why this phase matters: Retraining efficient posture and head-neck control reduces cervicogenic headache triggers and improves the quality of balance input your brain receives. (AAPM&R KnowledgeNow; DrAlexJimenez.com) PM&R KnowledgeNow+1
Phase 3: Build capacity and prevent contractures (Weeks 6–12)
-
Aerobic interval walks or cycling: 1–2 minutes easy / 1 minute moderate for 20 minutes; progress total time weekly.
-
Loaded strength: Add bands or light dumbbells to rows, squats, deadlifts (hip hinge with neutral spine), and overhead presses (pain-free range).
-
Mobility circuits: Thoracic spine open-books, hip flexor and calf stretches, gentle neck range drills; 10–15 minutes most days.
-
Dual-task and agility: March while counting backward by 3s; step-overs with head turns; carry a light bag while walking and naming items in a category.
-
Contracture prevention plan: Daily stretching of any tight muscle groups, nighttime splinting if prescribed, and frequent position changes. (Physiopedia; NR Times) Physiopedia+1
Why this phase matters: Strength and mobility protect joints, reduce stiffness, and give you the endurance for real-world tasks—shopping, work, parenting—without flare-ups. (Crumley House; BIAA) crumleyhouse.com+1
Special focus: The neck-brain link
Head-neck trauma can disturb cervical joint receptors, muscles, and fascia. That altered input can increase dizziness, headaches, and poor balance. Restoring healthy cervical motion and muscle timing enhances the effectiveness of vestibular therapy. Chiropractic care—used alongside PT—can help realign vertebrae, reduce muscle tension, and improve posture mechanics so the brain gets clearer signals during movement. (DrAlexJimenez.com, 2025; Cognitive FX, n.d.; AAPM&R KnowledgeNow, n.d.; Impact Medical Group, 2024) Impact Medical Group+3El Paso, TX Doctor Of Chiropractic+3CognitiveFX USA+3
Dr. Alexander Jimenez’s clinical observations (dual-scope chiropractic + NP)
From Dr. Jimenez’s clinical notes and patient education resources:
-
Start with safety and screening. Red flags (neurologic deficits, worsening severe headache, vision loss, suspected instability) = immediate medical work-up. (DrAlexJimenez.com, 2025) El Paso, TX Doctor Of Chiropractic
-
Gentle first, then progressive. Many patients tolerate joint mobilization before high-velocity adjustment and progress only when muscle guarding subsides and range of motion improves. (DrAlexJimenez.com, 2025) El Paso, TX Doctor Of Chiropractic
-
Posture and breath drive mobility. Teaching rib-pelvis stacking and diaphragmatic breathing helps reduce neck overuse and alleviates symptoms during balance drills. (DrAlexJimenez.com, 2025) El Paso, TX Doctor Of Chiropractic
-
Integrative plan matters. Combining spinal care, soft tissue therapy, vestibular-ocular rehab, strength training, and nutrition/sleep strategies improves adherence and outcomes. (DrAlexJimenez.com, 2025) El Paso, TX Doctor Of Chiropractic
Managing pain without losing motion
-
Keep moving in a safe zone. Movement supports fluid exchange and nutrient delivery; complete rest can worsen stiffness and tolerance to activity. (BIAA; MSKTC) Brain Injury Association of America+1
-
Treat the neck. Many post-TBI headaches are neck-related. Addressing cervical mechanics can reduce headache frequency and enable better exercise participation. (AAPM&R KnowledgeNow; Defrin et al., 2014) PM&R KnowledgeNow+1
-
Graded exposure works. Increase time, load, and complexity slowly, tracking symptoms to stay under your personal threshold. (Cognitive FX) CognitiveFX USA
What success looks like
-
Longer, steadier walks with fewer stumbles.
-
Easier head turns while walking or driving (after formal clearance).
-
Less neck tightness and fewer headaches.
-
More flexible hips, shoulders, and thoracic spine—with better posture in photos and mirrors.
-
The ability to carry groceries, climb stairs, or work a full shift with less crash afterward. (BIAA; Headway; MSKTC) Brain Injury Association of America+2headway.org.uk+2
Safety checklist (when to stop and call your clinician)
-
Worsening severe headache or new neurologic symptoms
-
Repeated vomiting, slurred speech, seizures, fainting
-
Neck instability, electric-shock sensations, or arm/leg weakness
-
Sudden vision loss or double vision
-
Significant new dizziness that does not settle with rest (Adapted from standard concussion safety guidance and clinical practice.) (MSKTC; AAPM&R KnowledgeNow) MSKTC+1
Frequently asked questions
Q: Can chiropractic care “fix” a TBI?
A: No. Chiropractic care does not heal the brain injury itself. But it can relieve neck-related pain, improve joint movement, posture, and sensorimotor input. That often makes physical therapy easier and safer, supporting your brain’s ability to adapt. (Impact Medical Group, 2024; DrAlexJimenez.com, 2025) Impact Medical Group+1
Q: I only have mild dizziness and tightness—do I still need help?
A: Yes. Small changes in gait and balance can be significant for reducing fall risk and improving confidence. Early treatment leads to better long-term mobility. (BIAA, n.d.) Brain Injury Association of America
Q: How do I prevent contractures?
A: Move often, stretch daily, change positions frequently, and follow your therapist’s splinting/positioning plan if prescribed. (Physiopedia; NR Times) Physiopedia+1
Simple home routine (after your clinician clears you)
10–20 minutes, 4–6 days/week. Stop if symptoms spike.
-
Breathing + posture (2–3 min): Nose breathing, gentle rib drop, tall spine.
-
Neck range (pain-free): Small nods, slow rotations (10–15 reps).
-
Scapular rows with band: 2×10–12.
-
Sit-to-stand: 2–3×8–12.
-
Tandem balance (near a counter): 2×20–30 sec; add small head turns as tolerated.
-
Walk 8–15 minutes at a pace you can talk through.
-
Stretch 5–8 minutes: Chest, hip flexor, calves; finish with 1 minute of gentle neck stretches.
(PT and chiropractic can personalize progressions.) (BIAA; Cognitive FX; DrAlexJimenez.com) Brain Injury Association of America+2CognitiveFX USA+2
The big picture: restore motion, feed the brain
-
Movement delivers oxygen and nutrients and helps regulate cerebrospinal fluid.
-
Reducing neck-driven pain and improving posture make balance retraining more effective.
-
Preventing stiffness and contractures keeps options open for future progress.
-
Consistent, graded practice—not “hero workouts”—rebuilds resilience. (BIAA; Headway; Physiopedia) Brain Injury Association of America+2headway.org.uk+2
Final thoughts
Recovering mobility and flexibility after a head injury takes time, but it is possible to rebuild. A sensible plan pairs medical safety with steady progression: easing pain and guarding, restoring joint motion, retraining balance and gait, and maintaining consistent practice. Chiropractic and integrative care, when coordinated with your therapy team, can address neck and spine contributors to dizziness, headaches, and posture strain, allowing your brain to receive clearer signals and your body to move with less effort. (BIAA; MSKTC; DrAlexJimenez.com) Brain Injury Association of America+2MSKTC+2
References
Brain Injury Association of America. (n.d.). Physical therapy and brain injury recovery. https://biausa.org/public-affairs/media/physical-therapy-and-brain-injury Brain Injury Association of America
Brain Injury Association of America. (n.d.). Slight changes in walking and balance after traumatic brain injury. https://biausa.org/professionals/research/tbi-model-systems/slight-changes-in-walking-and-balance-after-traumatic-brain-injury Brain Injury Association of America
Brain Injury Canada. (n.d.). Mobility. https://braininjurycanada.ca/en/effects-brain-injury/physical/mobility/ braininjurycanada.ca+1
Clinical Pain Advisor. (2017). Chronic pain associated with traumatic brain injury: Causes and management. https://www.clinicalpainadvisor.com/features/chronic-pain-associated-with-traumatic-brain-injury-causes-and-management/ clinicalpainadvisor.com
Cognitive FX. (n.d.). A patient’s guide to TBI physical therapy. https://www.cognitivefxusa.com/blog/tbi-physical-therapy CognitiveFX USA
Crumley House. (n.d.). The power of movement: How physical training supports traumatic brain injury recovery. https://crumleyhouse.com/blog_physical_training/ crumleyhouse.com
Defrin, R., et al. (2014). Chronic post-traumatic headache: Clinical findings and mechanisms. The Journal of Headache and Pain. https://pmc.ncbi.nlm.nih.gov/articles/PMC4062350/ PMC
Headway – the brain injury association. (n.d.). Physical effects of brain injury. https://www.headway.org.uk/about-brain-injury/individuals/effects-of-brain-injury/physical-effects-of-brain-injury/ headway.org.uk
Impact Medical Group. (2024, June 26). Can chiropractic care help with mild traumatic brain injuries? https://www.impactmedicalgroup.com/2024/06/26/can-chiropractic-care-help-with-mild-traumatic-brain-injuries/ Impact Medical Group
Model Systems Knowledge Translation Center (MSKTC). (2018). Understanding TBI: Part 2 – Brain injury impact on individuals’ functioning. https://msktc.org/tbi/factsheets/understanding-tbi-part-2-brain-injury-impact-individuals-functioning MSKTC
Moon, D., et al. (2022). Disorders of movement due to acquired and traumatic brain injury. Tremor and Other Hyperkinetic Movements. https://pmc.ncbi.nlm.nih.gov/articles/PMC9493170/ PMC
Neuro Rehab Times. (2024). Physiotherapy in post-TBI rehab (NR Notes). https://nrtimes.co.uk/nr-notes-physiotherapy-in-post-tbi-rehab/ nrtimes.co.uk
Pinnacle Health Chiropractic. (n.d.). Six ways chiropractic care supports healing after TBI. https://www.pinnaclehealthchiro.com/blog/six-ways-chiropractic-care-supports-healing-after-tbi Pinnacle Health Chiropractic
Physiopedia. (n.d.). Contracture management for traumatic brain injury. https://www.physio-pedia.com/Contracture_Management_for_Traumatic_Brain_Injury Physiopedia
Dr. Alexander Jimenez – clinical resources (dual-scope DC, APRN, FNP-BC)
DrAlexJimenez.com. (2025). Traumatic brain injury: Understanding the long-term effects. https://dralexjimenez.com/traumatic-brain-injury-understanding-the-long-term-effects/ El Paso, TX Doctor Of Chiropractic
DrAlexJimenez.com. (2025). Finding hidden TBI symptoms: Signs you might miss. https://dralexjimenez.com/finding-hidden-tbi-symptoms-signs-you-might-miss/ El Paso, TX Doctor Of Chiropractic
DrAlexJimenez.com. (2025). TBI toxicity after head injuries: An integrative plan. https://dralexjimenez.com/tbi-toxicity-after-head-injuries-an-integrative-plan/ El Paso, TX Doctor Of Chiropractic
DrAlexJimenez.com. (2023). Head pressure. https://dralexjimenez.com/head-pressure/ El Paso, TX Doctor Of Chiropractic
DrAlexJimenez.com. (2025). Rehabilitation exercises after head injuries — step-by-step plan. https://dralexjimenez.com/rehabilitation-exercises-after-head-injuries-step-by-step-plan/amp/ El Paso, TX Doctor Of Chiropractic
American Academy of Physical Medicine & Rehabilitation (AAPM&R). (n.d.). Post-traumatic headache. https://now.aapmr.org/postconcussion-headache/ PM&R KnowledgeNow
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Mobility & Flexibility After Head Injuries Recovery Tips" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics