Hidden Traumatic Brain Injuries: How Chiropractors and Nurse Practitioners Find What Others Miss

Many mild and moderate traumatic brain injuries (TBIs) are missed at first; a careful history, targeted questions, and a coordinated plan led by chiropractic care and nurse practitioner (NP) oversight can uncover hidden cognitive, emotional, sensory, sleep, and movement problems and guide safe, step-by-step recovery.
Why hidden TBIs are easy to miss
A traumatic brain injury is not always obvious. People can look “fine” on the outside while struggling with headaches, concentration problems, irritability, fatigue, light or sound sensitivity, and sleep changes that start days or weeks later. When symptoms develop slowly, busy clinics may not connect them to the original injury, and brief visits often overlook subtle clues that family members notice first. That’s why a complete history and the right screening questions are essential at every follow-up after a fall, car crash, sports hit, or blast exposure. (BrainLine, 2018; Mayo Clinic, n.d.) BrainLine+1
Legal and military health sources consistently warn that recognition is critical because many TBI symptoms are “invisible.” Patients, loved ones, and clinicians must watch for mood swings, irritability, depression, behavior changes, and sleep problems—especially in the first days and weeks. If these are missed, people can suffer longer and face ongoing work, school, and relationship problems that were preventable with timely care. (Hanscom AFB, 2017.) hanscom.af.mil
The “right questions” that uncover hidden symptoms
A careful interview by a chiropractor or nurse practitioner can reveal patterns that quick checklists miss. In addition to standard injury questions (what, when, where), ask:
-
Cognition: Since the incident, have you forgotten simple tasks? Lose your place mid-conversation? Read the same line twice? (BrainLine, 2018.) BrainLine
-
Emotions and behavior: Are you more irritable, anxious, or down than usual? Do small hassles make you very angry? Have others noticed changes? (Mayo Clinic, n.d.; Hanscom AFB, 2017.) Mayo Clinic+1
-
Sensory changes: Any new ringing in the ears, light sensitivity, blurred vision, or a change in smell or taste (for example, a “metallic” taste or food not tasting right)? (BrainLine, 2018; Fisher Stark, 2021.) BrainLine+1
-
Headache and fatigue: Do you wake with headaches? Do they worsen with screens or busy places? How is your energy across the day? (Mayo Clinic, n.d.) Mayo Clinic
-
Sleep: Trouble falling asleep, staying asleep, or sleeping too much? Non-refreshing sleep? (BrainLine, 2018; Mayo Clinic, n.d.) BrainLine+1
-
Balance and coordination: Any dizziness, unsteadiness, veering, or near-falls? (BrainLine, 2018.) BrainLine
-
Neck and jaw symptoms: Neck stiffness, pain, or clicking; jaw clenching; headaches starting at the base of the skull—clues to cervicogenic drivers that aggravate TBI symptoms. (NWHSU, n.d.; Denver Chiropractic, n.d.) Northwestern Health Sciences University+1
These targeted questions are quick, patient-friendly, and powerful. They open the door to a focused exam and a plan that treats both the brain and the musculoskeletal system that supports it.
Common symptom clusters to expect (and not overlook)
Cognitive changes: slow thinking, short-term memory issues, word-finding problems, difficulty with multitasking, and mental fatigue. (BrainLine, 2018.) BrainLine
Emotional and behavioral shifts: irritability, anger, anxiety, low mood, mood swings, and feeling “not like myself.” Loved ones often notice these first. (Hanscom AFB, 2017; Mayo Clinic, n.d.) hanscom.af.mil+1
Sensory symptoms: blurred vision, eyes that tire quickly, ringing in the ears, loss or change of smell/taste, light/sound sensitivity. (BrainLine, 2018; Fisher Stark, 2021.) BrainLine+1
Headache, sleep, fatigue: persistent or worsening headaches; insomnia or oversleeping; daytime drowsiness; and low energy. (Mayo Clinic, n.d.; BrainLine, 2018.) Mayo Clinic+1
Balance and movement: dizziness, vertigo, unsteadiness, slowed coordination; often linked with neck injuries that occur at the same time. (BrainLine, 2018; Denver Chiropractic, n.d.) BrainLine+1
An integrative care model: chiropractic + nurse practitioner leadership
TBIs often coexist with neck sprains, joint restrictions, soft-tissue injuries, and vestibular/oculomotor dysfunction. A coordinated plan led by a chiropractor and a nurse practitioner (NP) can stabilize both neural and musculoskeletal systems while screening for medical risks.
-
What the chiropractor leads:
-
Spinal and rib adjustments (applied judiciously, with safety screening) to improve joint motion and reduce cervicogenic headache drivers.
-
Soft-tissue therapies (myofascial techniques) to down-regulate muscle guarding and improve blood flow.
-
Neck-centric exercise progressions (deep neck flexors, scapular control), vestibular and oculomotor drills (gaze stabilization, smooth pursuit), and balance rehab (BESS-informed).
-
Pacing and graded exposure to everyday tasks and screen time.
Chiropractors in rehab settings commonly support neck-related pain, dizziness, and posture/movement issues that amplify concussion symptoms, and can collaborate on vestibular and vision-related strategies when trained to do so. (NWHSU, n.d.; BMC Chiropractic & Manual Therapies, 2018.) Northwestern Health Sciences University+1
-
-
What the NP leads:
-
Medical screening and red-flag triage, medication review, sleep strategies, headache management, and referrals for imaging, neuropsychology, ENT/vestibular, ophthalmology, or endocrinology when needed.
-
Monitoring for secondary injury risks (e.g., hypoxemia, blood pressure spikes in severe cases), patient and family education, and coordination across specialties.
-
Mental health support (screening for depression/anxiety), plus metabolic care (nutrition, hydration, and—when appropriate—monitoring endocrine changes seen after some TBIs). (MDPI—J Clin Med, 2024.) MDPI
-
Bottom line: combining hands-on musculoskeletal care with medical oversight and symptom-specific rehab meets patients where they are and adapts care as the brain heals. This is how many integrated clinics, including those led by dual-scope providers like Dr. Alexander Jimenez, DC, APRN, FNP-BC, structure stepwise, patient-centered TBI care. (Jimenez, n.d.) HML Functional Care
How chiropractic care fits—safely and specifically
Chiropractic care is complementary in TBI recovery. The focus is not on “fixing the brain” directly but on:
-
reducing cervicogenic headache and dizziness contributors,
-
improving sensorimotor control of the neck and upper back,
-
easing muscle tension that amplifies symptoms, and
-
guiding graded vestibular/oculomotor retraining and balance work in collaboration with the team.
Clinical resources describe potential benefits such as improved circulation, better neck alignment, and reduced headache/neck pain—always within a measured, individualized plan. (Denver Chiropractic, n.d.; Pinnacle Health Chiropractic, 2025; Apex Chiropractic, 2022; NWHSU, n.d.) Northwestern Health Sciences University+3Denver Integrated Spine Center+3pinnaclehealthchiro.com+3
Safety note: high-velocity adjustments are not automatically indicated after head/neck trauma. A skilled chiropractor performs thorough screening (neurologic, vascular, red-flag review) and uses gentler mobilization or instrument-assisted methods when appropriate, coordinating with the NP and the wider team. (BMC Chiropractic & Manual Therapies, 2018.) BioMed Central
Nurse practitioner supervision that protects the brain
In acute and subacute TBI, nurses and NPs play a central role in preventing secondary injury (the cascade of swelling, hypoperfusion, hypoxemia, and metabolic stress that worsens outcomes). While this scoping review focuses on critical care, its principles inform outpatient vigilance: monitor neurologic status, oxygenation, temperature, sleep, blood pressure, and red flags, and involve family in observation and support. (J Clin Med, 2024.) MDPI
For outpatient recovery, NPs:
-
coordinate neuropsychological testing, vestibular/vision care, and mental-health support;
-
manage sleep, headache, and mood symptoms;
-
guide return-to-work/school/sport progression;
-
counsel on hydration, nutrition, and pacing to reduce post-concussive symptom flares. (Mayo Clinic, n.d.; J Clin Med, 2024.) Mayo Clinic+1
High-level diagnostic tools and assessments—from basic to sophisticated
Use the least invasive tests that answer the current clinical question, and scale up only when needed.
Level 1: Basic bedside tools (early visits and primary care/rehab settings)
-
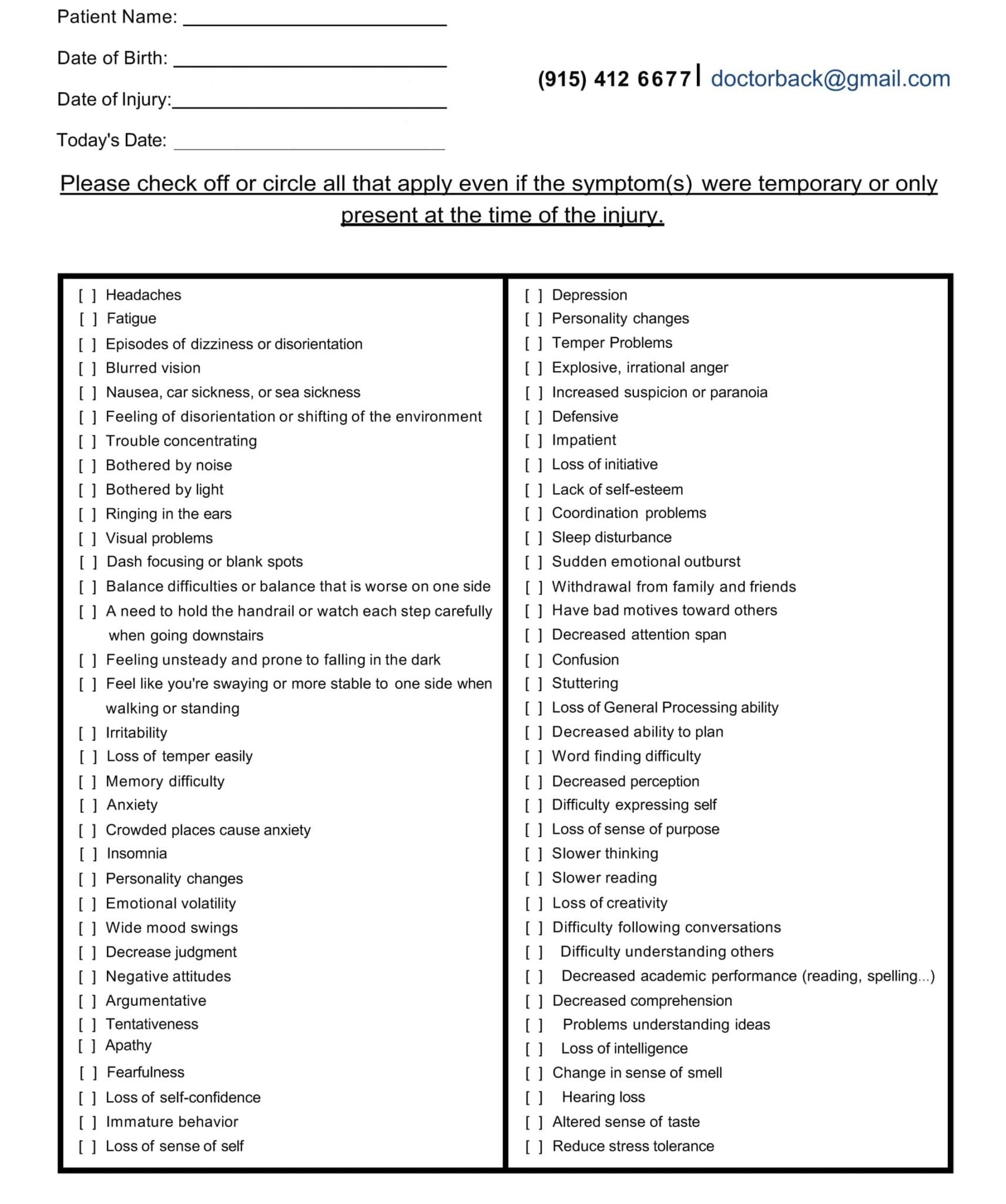
Detailed history + symptom checklists: Post-Concussion Symptom Scale (PCSS), Rivermead, sleep and mood screens.
-
Neurologic and cranial nerve exam; cervical exam (range of motion, segmental tenderness, myofascial trigger points).
-
Cognitive screens: MoCA or MMSE (brief).
-
Balance tests: Romberg/tandem gait; BESS for postural stability.
-
Vestibular/ocular-motor screen: VOMS (smooth pursuit, saccades, convergence, VOR).
-
Red-flag screen for severe TBI signs (worsening headache, seizures, focal weakness, repeated vomiting, unequal pupils, drainage from nose/ears, inability to awaken). (BrainLine, 2018; Mayo Clinic, n.d.) BrainLine+1
Level 2: Focused clinic testing (if symptoms persist beyond 1–2 weeks or are complex)
-
Neuropsychological testing for attention, memory, processing speed, and executive function (paper-and-pencil or computerized).
-
Vestibular/audiology: VNG, VEMP, dynamic visual acuity.
-
Vision/oculomotor: optometry/neuro-ophthalmology assessment (convergence, accommodation).
-
Computerized posturography for balance strategies; instrumented gait analysis in some centers.
-
Autonomic testing (e.g., HRV trends) if dysautonomia suspected;
-
Sleep evaluation and actigraphy when insomnia or hypersomnia drives daytime symptoms. (BrainLine, 2018; BMC Chiropractic & Manual Therapies, 2018.) BrainLine+1
Level 3: Advanced studies (ordered selectively by an NP/physician)
-
Imaging for red flags or prolonged deficits:
-
CT in acute settings for suspected intracranial bleeding or skull fracture.
-
MRI when symptoms persist or focal deficits are present; consider sequences such as SWI for microhemorrhages and DTI for white-matter tract changes (availability varies).
-
-
Electrophysiology: EEG for seizures; qEEG/evoked potentials in select cases.
-
Functional and metabolic imaging (selected cases, specialty centers): fMRI, SPECT/PET for persistent cognitive deficits when other tests are inconclusive.
-
Endocrine evaluation (if fatigue, libido change, temperature dysregulation, or growth/weight changes suggest pituitary involvement). (Mayo Clinic, n.d.) Mayo Clinic
Key point: start simple, escalate only when needed, and always tie test selection to the patient’s current symptoms and goals. (BMC Chiropractic & Manual Therapies, 2018.) BioMed Central
A step-by-step integrative plan (example pathway)
Stage 1 (Days 1–7): Calm the system and ensure safety
NP: rule out red flags; manage headache, sleep, and nausea; provide clear return-precautions and pacing guidelines.
Chiropractor: gentle soft-tissue work; no high-velocity neck manipulation in the acute phase; start breathing drills, light isometrics, and postural decompression; educate on neck positioning and screen breaks. (Mayo Clinic, n.d.; BMC Chiropractic & Manual Therapies, 2018.) Mayo Clinic+1
Stage 2 (Weeks 2–4): Restore motion, balance, and visual-vestibular control
Chiropractor: progress to low-amplitude mobilizations or instrument-assisted adjustments if screening is clear; add gaze stabilization (VOR x1/x2), smooth pursuit drills, graded balance work, scapular/neck endurance, and walking programs.
NP: monitor sleep/mood; consider neuropsych or vestibular/vision referrals if symptoms persist; manage medications carefully and ensure hydration and nutrition. (NWHSU, n.d.; J Clin Med, 2024.) Northwestern Health Sciences University+1
Stage 3 (Weeks 4–8+): Build resilience and return to roles
Team: advance strengthening and dual-task drills (movement + attention), increase community exposures (stores, traffic, classrooms), and add workplace/school simulations; review driving readiness when symptoms are stable.
Outcome tracking: repeat PCSS/BESS; ensure symptoms do not worsen >2 points with each step; if they do, step back and retry after rest. (BrainLine, 2018.) BrainLine
Targeted therapies that support cognition throughout the body
-
Cervicogenic headache relief: Addressing stiff upper cervical segments, suboccipital tightness, and scapular weakness reduces afferent “noise” that can drive headaches and brain fog. (NWHSU, n.d.; Pinnacle Health Chiropractic, 2025.) Northwestern Health Sciences University+1
-
Balance and gaze control: Vestibular drills and oculomotor training improve stability and reduce motion sensitivity, making reading, driving, and crowded places more tolerable. (BrainLine, 2018.) BrainLine
-
Soft-tissue therapy and movement: Myofascial release and graded exercise lower muscle guarding and improve circulation, helping energy and mental clarity. (Denver Chiropractic, n.d.; Apex Chiropractic, 2022.) Denver Integrated Spine Center+1
-
Lifestyle and metabolic support: NPs guide sleep timing, hydration, and anti-inflammatory nutrition; monitor mood and stress; and refer for counseling when needed. (J Clin Med, 2024; Mayo Clinic, n.d.) MDPI+1
Red-flag checklist (seek immediate medical care)
-
Worsening or severe headache, repeated vomiting, unequal pupil size, seizures, weakness or numbness in limbs, slurred speech, clear fluid from nose/ears, or inability to awaken. (BrainLine, 2018; Mayo Clinic, n.d.) BrainLine+1
How this model looks in practice
Integrated clinics that combine chiropractic care with NP supervision routinely:
-
Screen thoroughly, ask the right questions, and use targeted bedside tests;
-
Stabilize the neck and soft tissues that amplify brain symptoms;
-
Rebuild vestibular, visual, and balance control through stepwise drills;
-
Manage sleep, mood, and metabolic health with education and medical oversight;
-
Escalate testing only when needed, and coordinate referrals to specialty care.
Stakeholders in neurorehabilitation prefer chiropractors who are patient-centered, safe, collaborative, and evidence-informed—fitting naturally into teams that include medicine, nursing, therapy, vision, and audiology. (BMC Chiropractic & Manual Therapies, 2018.) BioMed Central
Take-home points for patients and families
-
Many TBIs are missed early; if something feels off in the days or weeks after a head/neck injury, say so and ask for a thorough TBI screen. (BrainLine, 2018.) BrainLine
-
Subtle symptoms—concentration problems, anger or irritability, and changes in taste or smell—are common and meaningful. (Mayo Clinic, n.d.; Fisher Stark, 2021.) Mayo Clinic+1
-
An integrative plan pairing chiropractic therapy (for musculoskeletal and vestibular drivers) with NP supervision (for medical, mental, and metabolic care) offers a safe, comprehensive path forward. (NWHSU, n.d.; J Clin Med, 2024.) Northwestern Health Sciences University+1
Conclusion
Hidden TBIs are common—but they do not have to steal months or years of quality life. Chiropractors and nurse practitioners can detect what others miss by taking a careful history and asking targeted questions about cognition, emotions, senses, sleep, balance, and neck function. With patient-centered teamwork, they can treat the full picture using spine and soft-tissue care, movement and vestibular training, and medical oversight for sleep, mood, headache, and metabolism. If your symptoms persist, push for a proper TBI evaluation and a step-by-step, integrated care plan—because recovery is real, and it starts with being seen. (BrainLine, 2018; Mayo Clinic, n.d.; BMC Chiropractic & Manual Therapies, 2018; J Clin Med, 2024.) MDPI+3BrainLine+3Mayo Clinic+3
References
-
BrainLine. (2018). Symptoms of Traumatic Brain Injury (TBI). BrainLine
-
Denver Chiropractic. (n.d.). Mild Traumatic Brain Injury—Can a Chiropractor Help?. Denver Integrated Spine Center
-
Fisher Stark, P.A. (2021, January 23). Hidden Signs of a Serious Head Injury (Traumatic Brain Injury Symptoms). Fisher Stark P.A.
-
Hanscom Air Force Base. (2017, March 10). TBI recognition critical to treating invisible wounds. hanscom.af.mil
-
Mayo Clinic. (n.d.). Traumatic brain injury—Symptoms & causes. Mayo Clinic
-
Northwest Health Sciences University (NWHSU). (n.d.). Chiropractic and traumatic brain injuries. Northwestern Health Sciences University
-
Pinnacle Health Chiropractic. (2025). Six ways chiropractic care supports healing after TBI. pinnaclehealthchiro.com
-
Apex Chiropractic. (2022, August 18). 3 Benefits of Chiropractic Care Following a Traumatic Brain Injury. Apex Chiropractic
-
Salsbury, S. A., Vining, R. D., Gosselin, D., & Goertz, C. M. (2018). Be good, communicate, and collaborate: a qualitative analysis of stakeholder perspectives on adding a chiropractor to the multidisciplinary rehabilitation team. Chiropractic & Manual Therapies, 26(1), 29. BioMed Central
-
Figueiredo, R., Castro, C., & Fernandes, J. B. (2024). Nursing interventions to prevent secondary injury in critically ill patients with traumatic brain injury: A scoping review. Journal of Clinical Medicine, 13(8), 2396. MDPI
-
Jimenez, A. (n.d.). dralexjimenez.com. Clinical observations from a dual-scope (DC + APRN, FNP-BC) practice. HML Functional Care
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Hidden Traumatic Brain Injuries: Recognizing the Signs" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



