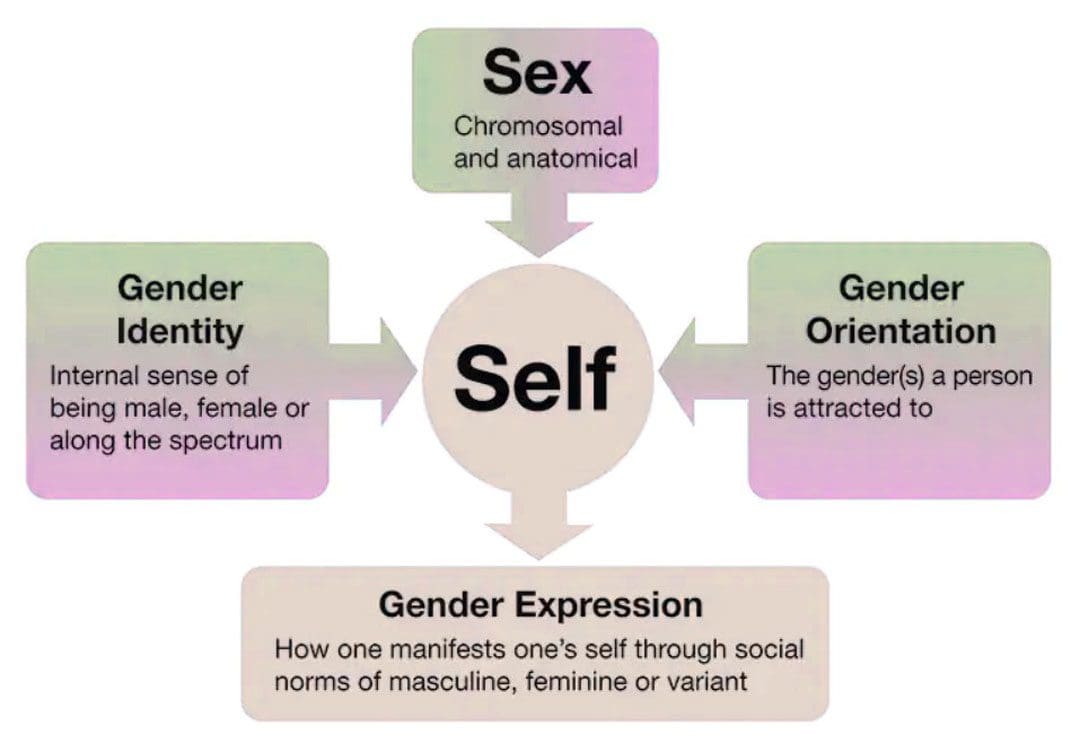
Gender transitioning is the process of affirming and expressing an individual’s internal sense of gender rather than the one assigned at birth. How can learning the aspects of gender and gender transitioning help support the LGBTQ+ community?
Gender Transitioning
Gender transitioning or gender affirmation is a process through which transgender and gender-nonconforming individuals align their internal gender identity with their external gender expression. It can be described as a binary – male or female – but can also be non-binary, meaning an individual is neither exclusively male nor female.
- The process can involve aesthetic appearances, changes in social roles, legal recognitions, and/or physical aspects of the body.
- Social affirmation – dressing differently or coming out to friends and family.
- Legal affirmation – changing name and gender on legal documents.
- Medical affirmation – using hormones and/or surgery to change certain physical aspects of their body.
- Transgender individuals can pursue some or all of these.
Barriers
Gender transitioning can be obstructed by various barriers that can include:
- Cost
- Lack of insurance
- Lack of family, friends, or partner support.
- Discrimination
- Stigma
Addressing All Aspects
The process does not have a specific timeline and is not always linear.
- Many transgender and gender-nonconforming individuals prefer gender affirmation to gender transitioning because transitioning is often taken to mean the process of medically transforming the body.
- An individual does not have to undergo medical treatment to affirm their identity, and some transgender people avoid hormones or gender-affirming surgery.
- Transitioning is a holistic process that addresses all aspects of who a person is inwardly and outwardly.
- Certain aspects of transitioning may be more important than others, like changing one’s name and gender on their birth certificate.
- Reevaluation and revision of gender identity can be continual rather than a step-by-step, one-way process.
Exploring Gender Identity
Gender transitioning often starts in response to gender dysphoria which describes the constant sense of uneasiness that occurs when the gender an individual was assigned at birth does not match how they experience or express their gender internally.
- Some individuals have experienced symptoms of gender dysphoria as early as 3 or 4 years of age. (Selin Gülgöz, et al., 2019)
- Gender dysphoria can be largely informed by the culture that surrounds the individual, specifically in cultures where strict codes determine what is masculine/male and feminine/female.
Unease Expressed in Different Ways
- Dislike of one’s sexual anatomy.
- A preference for clothes typically worn by the other gender.
- Not wanting to wear clothes typically worn by their own gender.
- A preference for cross-gender roles in fantasy play.
- A strong preference for engaging in activities that are typically done by the other gender.
Dysphoria
- Gender dysphoria can fully emerge during puberty when awareness about how an individual’s body defines them creates internal distress.
- Feelings may be amplified when an individual is described as a tomboy, or a sissy, or is criticized and attacked for acting like a girl or acting like a boy.
- During puberty, the physical changes can cause long-standing feelings of not fitting in and may evolve into feelings of not fitting in their own body.
- This is when individuals can undergo a process referred to as internal transitioning and begin to change how they see themselves.
Gender transitioning/affirmation becomes the next step. Transitioning is not about changing or recreating oneself but about expressing their authentic self and asserting who they are socially, legally, and/or medically.
Social
Social transitioning involves how a person publicly expresses their gender. The transition can include:
- Changing pronouns.
- Using chosen name.
- Coming out to friends, family, coworkers, etc.
- Wearing new clothes.
- Cutting or styling hair differently.
- Changing mannerisms like moving, sitting, etc.
- Changing voice.
- Binding – strapping the chest to hide breasts.
- Wearing breast and hip prosthetics to accentuate feminine curvature.
- Packing – wearing a penile prosthesis to create a penile bulge.
- Tucking – tucking the penis to conceal a bulge.
- Playing certain sports
- Pursuing different lines of work.
- Participating in activities that might typically be seen as male or female.
Legal
Legal transitioning involves changing legal documents to reflect the individual’s chosen name, gender, and pronouns. This includes governmental and non-government documents that can include:
- Birth certificates
- Social Security ID
- Driver’s license
- Passport
- Bank records
- Medical and dental records
- Voter registration
- School ID
- Provisions allowing for changes can vary by state.
- Some states only allow changes if bottom surgery – genital reconstruction is performed.
- Others will allow the changes without any form of gender-affirming surgery.
- Other states have begun to offer an X-gender option for non-binary individuals. (Wesley M King, Kristi E Gamarel. 2021)
Medical
Medical transitioning typically involves hormone therapy to develop some of the male or female sex characteristics. It can also involve surgery to change certain physical aspects combined with hormone therapy.
- Hormone therapy assists individuals to physically look more like the gender they identify as.
- They can be used on their own and can also be used before gender-affirming surgery.
Hormone therapy takes two forms:
Transgender Men
- Testosterone is taken to help deepen the voice, increase muscle mass, promote body and facial hair, and enlarge the clitoris. (M S Irwig, K Childs, A B Hancock. 2017)
Transgender Women
- Estrogen is taken as well as testosterone blockers to redistribute body fat, increase breast size, reduce male-pattern baldness, and reduce testicle size. (Vin Tangpricha 1, Martin den Heijer. 2017)
Surgery
Gender affirmation surgery aligns an individual’s physical appearance to their gender identity. Many hospitals provide gender-affirming surgery through a transgender medicine department. Medical procedures include:
- Facial surgery – Facial feminization surgery.
- Breast augmentation – Increases breast size with implants.
- Chest masculinization – Removes contours of breast tissues.
- Tracheal shaving – Reduces the Adam’s apple.
- Phalloplasty – Construction of a penis.
- Orchiectomy – Removal of the testicles.
- Scrotoplasty – Construction of a scrotum.
- Vaginoplasty – Construction of a vaginal canal.
- Vulvoplasty – Construction of the outer female genitalia.
Roadblocks
- Transgender individuals are protected from public and private insurance discrimination under federal and state laws, including Medicare and Medicaid. (National Center for Transgender Equality. 2021)
- Medicaid programs in nine states do not cover gender-affirming medical treatments, and only Illinois and Maine offer comprehensive standard care recommended by the World Professional Association for Transgender Health/WPATH. (Kaiser Family Foundation. 2022)
- Medicare also has no consistent policy regarding the approval of gender-affirming surgery.
- It relies on precedents in individual states to direct whether a treatment is approved or not. (Center of Medicare and Medicaid Services. 2016)
- In private insurance, most providers have removed restrictions on gender-affirming care.
- Larger insurers like Aetna and Cigna typically cover a more comprehensive array of services, in full or part.
- Smaller insurers might not cover surgeries and only cover things like hormone therapy. (Transgender Legal Defense and Education Fund. 2023)
- Another roadblock is stigma and discrimination.
- Studies show that more than half of transgender individuals report being harassed or bullied in public. (National Center for Transgender Equality and National Gay and Lesbian Task Force. 2011)
- Others report family or partner disapproval as the main reason why they discontinue gender affirmation. (Jack L. Turban, et al., 2021)
If you know someone who is transgender or is considering transitioning, learning about gender and gender transitioning and how to be supportive is a great way to be an ally.
Enhancing Your Lifestyle
References
Gülgöz, S., Glazier, J. J., Enright, E. A., Alonso, D. J., Durwood, L. J., Fast, A. A., Lowe, R., Ji, C., Heer, J., Martin, C. L., & Olson, K. R. (2019). Similarity in transgender and cisgender children’s gender development. Proceedings of the National Academy of Sciences of the United States of America, 116(49), 24480–24485. https://doi.org/10.1073/pnas.1909367116
Irwig, M. S., Childs, K., & Hancock, A. B. (2017). Effects of testosterone on the transgender male voice. Andrology, 5(1), 107–112. https://doi.org/10.1111/andr.12278
Tangpricha, V., & den Heijer, M. (2017). Estrogen and anti-androgen therapy for transgender women. The Lancet. Diabetes & endocrinology, 5(4), 291–300. https://doi.org/10.1016/S2213-8587(16)30319-9
National Center for Transgender Equality. Know Your Rights in Health Care.
Kaiser Family Foundation. Update on Medicaid coverage of gender-affirming health services.
Center of Medicare and Medicaid Services. Gender dysphoria and gender reassignment surgery.
Transgender Legal Defense and Education Fund. Health insurance medical policies.
National Center for Transgender Equality and National Gay and Lesbian Task Force. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey.
Turban, J. L., Loo, S. S., Almazan, A. N., & Keuroghlian, A. S. (2021). Factors Leading to “Detransition” Among Transgender and Gender Diverse People in the United States: A Mixed-Methods Analysis. LGBT health, 8(4), 273–280. https://doi.org/10.1089/lgbt.2020.0437
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Gender Transitioning: Expressing and Affirming Gender Identity" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



