Do you feel:
- Perimenopausal?
- Inflammation in the joints?
- Alternating menstrual cycle lengths?
- Hot flashes?
- Hormonal imbalances?
If you are experiencing any of these situations, then you might be experiencing menopause and its symptoms.
When a woman hits their late forties and entering their early fifties, they go through the natural aging process known as menopause. Menopause is when a woman has not menstruated in about twelve consecutive months as well as can no longer become pregnant. With menopause comes uncomfortable symptoms like hot flashes, vaginal dryness, and hormones imbalance. For women, hormone imbalances can range from having too much or too little hormones in the body’s bloodstream. When menopause occurs, the loss of the ovarian function in a female’s body can have an impact on their skeletal health, causing osteoporosis in the joints.
Osteoporosis and Menopause
Surprisingly though, the hormone estrogen can play a role in the development of osteoarthritis and when a woman is under the menopausal phase. They can experience a decline in their estrogen levels, and osteoporosis will begin to wreak the bones and joints, causing chronic inflammation. Studies have found out that when estrogen hormones begin to change during healthy menopausal changes, they will begin to fluctuate then suddenly drop. They stated that estrogen helps prevent bones from getting weaker through the natural breakdown. Any fractures from accidents can cause pain, decreased mobility, and normal function of the female body due to osteoporosis.
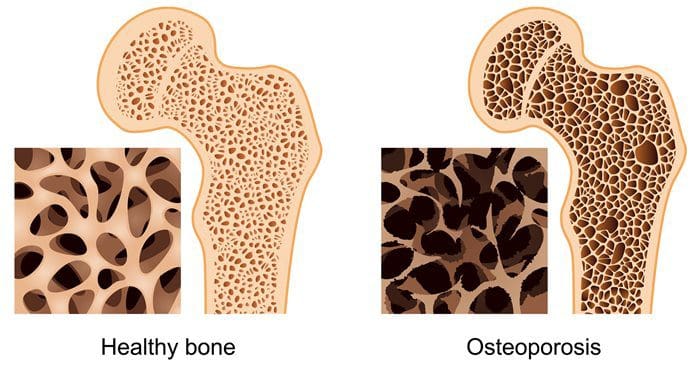
There is even more evidence that the fluctuation of estradiol that may even be more pronounced in the perimenopause and might not be able to correlate well with bone density and loss for the body. So, during the menopausal stage, the bone density will deteriorate when females have osteoporosis. There have been rumors that osteoporosis is something that a person should not have to worry because it only happens if there is a family history of osteoporosis. Sadly though, osteoporosis is a common bone disease, and having a family history of the disease can increase the chances. However, there are also other risk factors that can cause osteoporosis like:
- Excessive alcohol
- Amenorrhea
- Smoking
- Low body weight
Research shows that osteoporosis does start when a woman is at the start of the menopausal stage and has stopped ovulating, her monthly menstrual cycle stops. Her estrogen levels will dramatically stop, as well. It stated that women could have a total bone loss within the first ten years that follow menopause. When there is a lack of estrogen in the body due to menopause, bone density loss is much more significant and can cause fractures in the body. Studies have found out that local health care professionals will ask women about the amount of bone density that has been lost during their menopausal transition and when they begin. They even found out that the follicle-stimulating hormone in women has changed as well during their menopausal transition.
Bone Remodeling
Furthermore, studies found that over 20 American individuals are affected by osteoporosis, and this can lead to about 1.5 million bone fractures each year, thus making osteoporosis to be one of the leading public health problems. More studies even found that women would lose at least fifty percent of their trabecular bone, and about thirty percent of their cortical bone in their body will eventually be lost during the first ten years during their postmenopausal stage. Women must at least take vitamin D supplements to make sure that their bones are healthy and are not prone to bone loss or fractures.
There is information about why bone loss seems to accelerate after a woman’s menstrual cycle has ended and why bone remodeling can help replace the old bones that have been lost due to osteoporosis or due to fracture. Surprisingly though, bone remodeling is a process to replace old bones with new bones for the body, and it is consists of five phases. They are:
- Activation: During this phase of bone remodeling, osteoclasts are being recruited to the surface of the bone.
- Resorption: In this phase, the osteoclast is being generated into an acidic microenvironment on the surface of the bone, thus dissolving and resorbing the bone’s mineral content.
- Reversal: In this phase, the osteoclast then undergoes apoptosis and then is being recruited onto the bone’s surface.
- Formation: This is the last phase of bone remodeling as the osteoclast deposits collagen and then being mineralized to form a new bone in the body.
Conclusion
Menopause is a natural part of hormone levels to drop, and women cannot get pregnant any more. One of the most common signs that menopausal women encountered is osteoporosis. Osteoporosis is when bones become brittle and can break from falls or injury. Women need to take supplements for bone health so that way the bones and the body is functioning correctly. Some products are designed to help support the estrogen metabolism in both the female and male bodies as well as products to help support the hormonal balance and the normal menstruation for females in the reproductive age.
The scope of our information is limited to chiropractic, musculoskeletal, and nervous health issues or functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or disorders of the musculoskeletal system. Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900.
References:
Duggal, Neel. “What’s the Connection Between Menopause and Arthritis?” Healthline, 11 May, 2017, www.healthline.com/health/menopause/menopausal-arthritis.
Finkelstein, Joel S, et al. “Bone Mineral Density Changes during the Menopause Transition in a Multiethnic Cohort of Women.” The Journal of Clinical Endocrinology and Metabolism, The Endocrine Society, Mar. 2008, www.ncbi.nlm.nih.gov/pmc/articles/PMC2266953/.
Rodriguez, Diana, et al. “The Osteoporosis-Menopause Connection.” EverydayHealth.com, 16 Feb. 2016, www.everydayhealth.com/menopause/osteoporosis-and-menopause.aspx.
Rosen, Clifford, and Ramon Martinez. “Post Menopause and Osteoporosis.” Hormone Health Network, Mar. 2019, www.hormone.org/diseases-and-conditions/menopause/post-menopause-and-osteoporosis.
Sowers, MaryFran R, et al. “Amount of Bone Loss in Relation to Time around the Final Menstrual Period and Follicle-Stimulating Hormone Staging of the Transmenopause.” The Journal of Clinical Endocrinology and Metabolism, The Endocrine Society, May 2010, www.ncbi.nlm.nih.gov/pmc/articles/PMC2869543/.
Team, Penn Medicine. “Menopause And Osteoporosis: What’s The Connection? – Penn Medicine.” – Penn Medicine, 18 Mar. 2016, www.pennmedicine.org/updates/blogs/womens-health/2016/march/menopause-and-osteoporosis.
Tella, Sri Harsha, and J Christopher Gallagher. “Prevention and Treatment of Postmenopausal Osteoporosis.” The Journal of Steroid Biochemistry and Molecular Biology, U.S. National Library of Medicine, July 2014, www.ncbi.nlm.nih.gov/pmc/articles/PMC4187361/.
Modern Integrative Wellness- Esse Quam Videri
The University offers a wide variety of medical professions for functional and integrative medicine. Their goal is to inform individuals who want to make a difference in the functional medical fields with knowledgeable information that they can provide.
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Functional Endocrinology: Menopause and Osteoporosis" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



