When you visit a doctor office for a medical concern, the healthcare professional will perform a variety of diagnostic procedures to determine the source of your symptoms. The doctor will review the patient’s current symptoms and medical history as well as the patient’s results from a physical evaluation to diagnose an injury and/or underlying condition.
Once the healthcare professional has reviewed the patient’s current symptoms, medical history, and results from the physical evaluation, the doctor will make a list of the probable injuries and/or underlying conditions which may be causing the patient’s symptoms. This is the differential diagnosis. A differential diagnosis refers to the process of differentiating between two or more health issues which share similar signs and symptoms. The doctor will perform additional tests or assessments to rule out specific injuries and/or underlying conditions in order to reach a final diagnosis and follow-up with treatment.
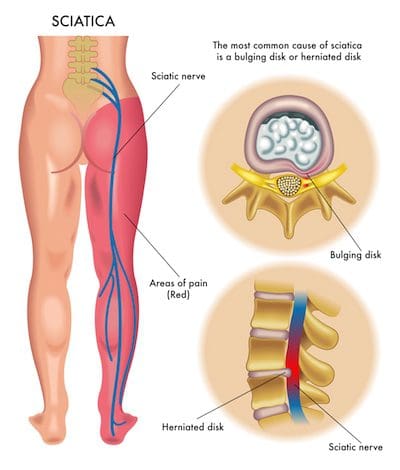
The differential diagnosis generally varies depending on the health issue. A variety of health issues can cause common symptoms which may make it challenging to determine the source of the pain and discomfort. Sciatica is a collection of symptoms rather than a single condition which can be a frequent symptom for many health issues. Sciatica is characterized as pain, tingling sensations, and numbness, due to compression or impingement along the length of the sciatic nerve.
Sciatica
The characteristic symptoms of sciatica can range from mild to severe where the sciatic nerve pain is described as a dull ache to pain or as a sharp, searing, or electric-like pain. Symptoms differ from one person to another. By way of instance, some people may experience shooting pain while some people may only experience tingling sensations and/or numbness.
The common symptoms of sciatica, also known as sciatic nerve pain, include:
- Radiating pain along the length of the sciatic nerve
- Discomfort, tingling sensations, and numbness
- Muscle weakness in the lower back, hips, legs, and feet
- A combination of pain, discomfort, tingling sensations and numbness
- Painful sensations on one or both sides of the human body
Sciatica commonly occurs when an underlying health issue results in the compression or impingement of the sciatic nerve in the lower back. A bulging or herniated disk is one of the most common causes of sciatica. However, a variety of other underlying health issues can cause sciatica and determining what causes sciatica is necessary for proper treatment. In part 1 of this article, we will demonstrate the differences between sciatica and other health issues with similar painful symptoms.
Degenerative Disc Disease
The intervertebral discs also referred to as spinal discs or intervertebral fibrocartilage, provide the padding required between the vertebrae of the spine. The intervertebral discs are an elastic structure made from fibrocartilage tissue. The intervertebral discs cushion the stress of the spine, bears weight, and also helps the spine bend and flex.
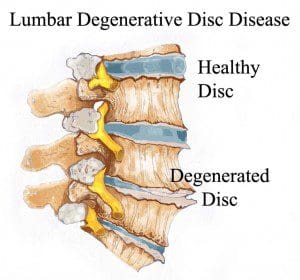
As people age, repeated daily stresses on the backbone and occasional trauma and/or injuries, including minor, undetected health issues, may ultimately damage the intervertebral discs in the back. Changes caused by damage may include:
- Decreased fluid: The intervertebral disks of a healthy young adult are made up of around 90 percent fluid. With age, the fluid material decreases, causing the disc to become thinner. The distance between each vertebra, in turn, becomes smaller and it makes them even less effective to function as a cushion or shock-absorber.
- Disc structure: Small tears or cracks can become larger in the outer layer of the disc. The soft and gelatinous material from the inner part may push through the disc, causing a bulging or ruptured disc. The disc may break into fragments.
If the vertebrae have less padding between them, the backbone also becomes less stable. To compensate, the human body builds osteophytes, or bone spurs, small bony structures which develop along the edge of bones. These structures can compress or impinge the spinal cord or nerve roots. These changes can cause painful symptoms and lead to fatigue.
The pain and discomfort can range from mild to severe and it may often be debilitating. It may result in osteoarthritis along with pain and stiffness. When degenerative disc disease affects the low back or the lumbar spine, the pain may radiate down the buttocks, hips, and thighs, into the knees and feet. There might also be tingling sensations and numbness, the collection of symptoms known as sciatica, caused due to the compression or impingement of the sciatic nerve.
Radiculopathy
The spine consists of 33 bones, best known as vertebrae, which shield the spinal cord from experiencing injury or trauma. Each vertebra is cushioned from each other with an intervertebral disk. This shields the vertebrae from rubbing over each other. When trauma or injury does occur, these intervertebral discs can become damaged and cause the compression or impingement of a nerve. Depending on which nerve is compressed, an individual can experience a variety of painful symptoms, including sciatica or sciatic nerve pain. Individuals can also develop radiculopathy seemingly without a cause.
Radiculopathy can ultimately develop due to a variety of injuries and/or aggravated conditions, including:
- Herniated discs, or when a disc protrudes, irritating the nerve root
- Sciatica
- Degenerative disc disease
- Bone spurs
- Tumors in the spine
- Osteoarthritis or spinal arthritis
- Spinal stenosis, or the narrowing of the spinal canal
- Compression fractures
- Spondylolisthesis, or when a vertebra slides over the vertebra beneath it
- Scoliosis brought on by an abnormal curve in the backbone
- Diabetes, caused by altered nerve blood flow
- Cauda equine syndrome, or a condition where nerve root compression affects the pelvic organs and lower extremities
Additional risk factors for developing radiculopathy include:
- Aging
- Being overweight or obese
- Poor posture
- Improper lifting methods and techniques
- Repetitive movements
- A family history of degenerative bone health issues
Individuals may experience painful symptoms in the low back, hips, and legs when nerve compression or impingement occurs in the lumbar spine or low back region of the spine. Lumbar radiculopathy is also commonly referred to as sciatica or sciatic nerve pain. Sciatica symptoms include pain, tingling sensations, and numbness along the length of the sciatic nerve. Occasionally, the nerve roots in charge of controlling the bowel and bladder may become irritated, resulting in bowel or bladder incontinence as well as loss of control. Other generalized symptoms associated with lumbar radiculopathy include:
- Sharp pain extending from the low back to the foot
- Sharp pain with sitting or coughing
- Weakness or numbness in the lower extremities
- Tingling sensations and numbness in the lower extremities
- Hypersensitivity, or sensitivity and reflex alterations
- Sharp pain radiating into the upper extremities
- Intense pain and discomfort with movements of the head and/or neck
Piriformis Syndrome
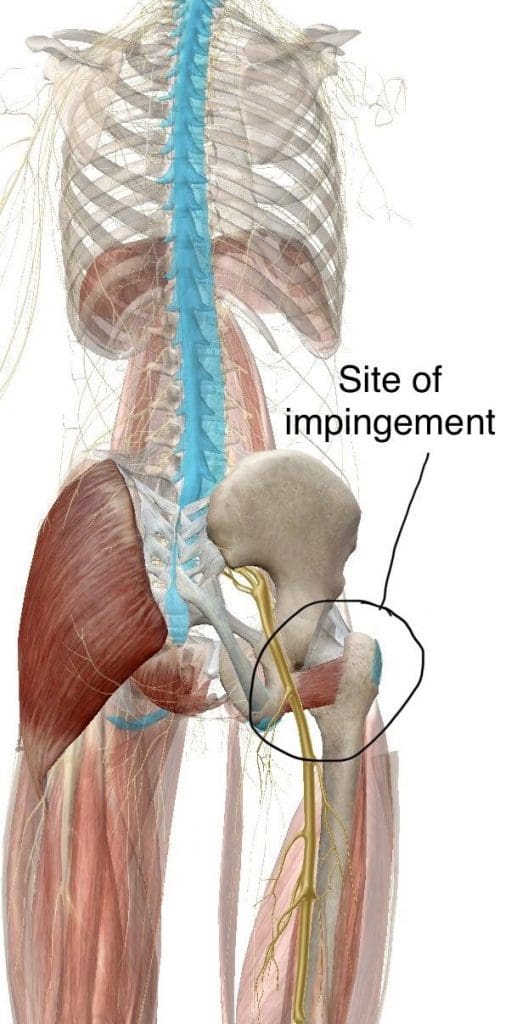
People with sciatic nerve pain, or sciatica, will often report experiencing pain and discomfort, tingling sensations, and numbness anywhere along the length of the sciatic nerve. The sciatic nerve is the longest and largest nerve in the human body, which travels from the lower back into the hip and buttocks, down into the thighs, knees, legs, and feet. People with sciatica, or sciatic nerve pain, may also experience another common health issue known as piriformis syndrome.
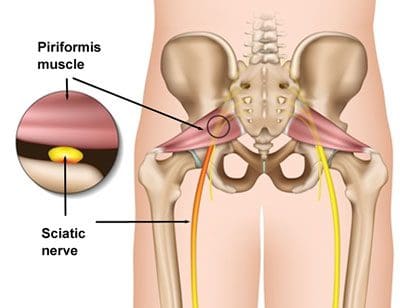
Piriformis syndrome can cause sciatica when a piriformis muscle spasm irritates the sciatic nerve. The piriformis is a muscle which extends from the front of the sacrum, the triangle-shaped bone between the two hipbones in the pelvis, across the sciatic nerve and into the top of the femur, the large bone in the upper leg. When an injury or underlying condition causes the piriformis muscle to compress or impinge the sciatic nerve due to inflammation, the end result is piriformis syndrome.
Sciatica is the most common symptom associated with piriformis syndrome. Other common symptoms associated with piriformis syndrome include tingling sensations and numbness, muscle tenderness, pain and discomfort while sitting or engaging in physical activities, and difficulty sitting comfortably. The pain and discomfort will generally manifest on one or both sides of the hips, buttocks, and thighs, where it will then radiate down the back of the leg, knees, and feet.
Facet Arthropathy
The facet joints are the joints which are found behind the spine to counterbalance the intervertebral discs found between the vertebrae of the spine. Over time, the natural aging process can cause the facet joints to deteriorate or wear down, causing facet joint arthritis or facet arthropathy. Individuals with facet arthropathy will experience low back pain as a dull ache on one or both sides of the lower back or lumbar spine which can worsen with standing, twisting, or bending backward.
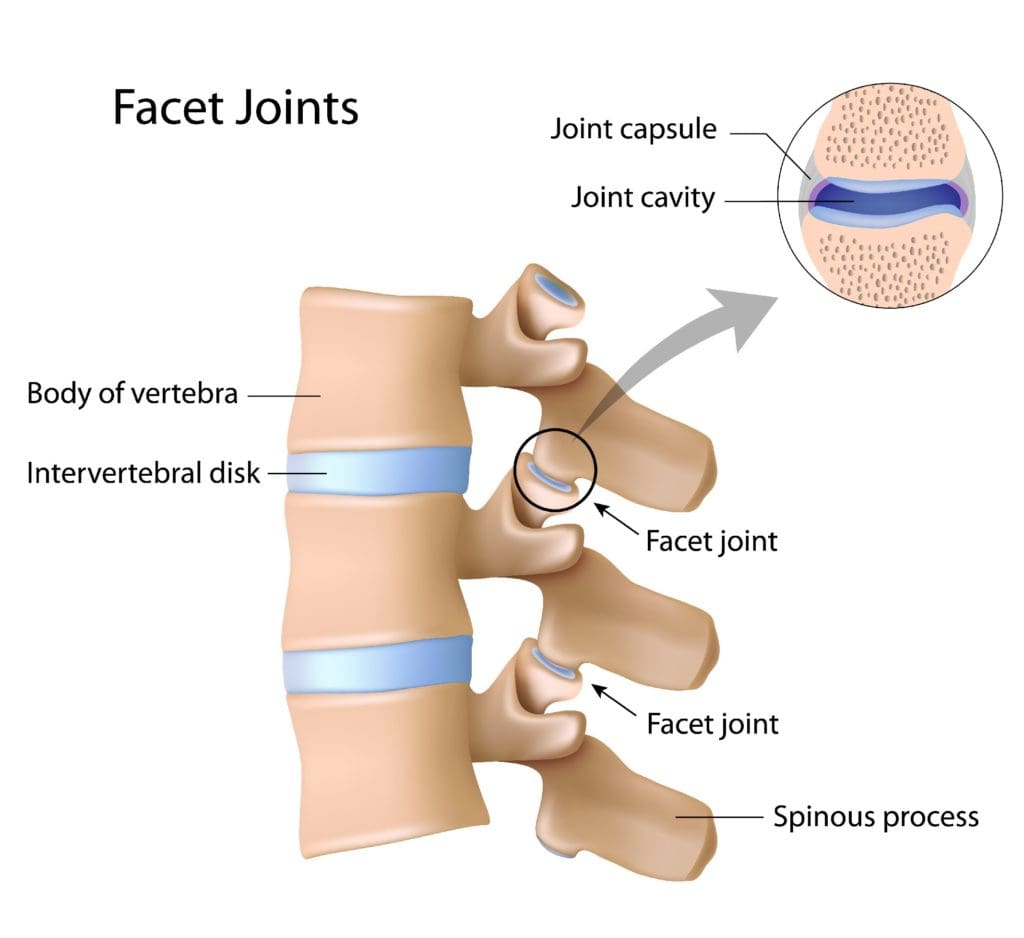
However, unlike the well-known signs and symptoms of sciatica, caused by the compression or impingement of the sciatic nerve in the lower back, facet arthropathy signs and symptoms generally don’t radiate down the buttocks, hips, and thighs, or into the legs and feet. However, the facet joint, in the same way as any other joint which has arthritis, can also become enlarged and add pressure on nerve roots, causing pain and discomfort to radiate down into the lower extremities.
Facet arthropathy may cause bone spurs, tiny bone outgrowths. Bone spurs can decrease the distance available between nerve roots, causing a health issue known as spinal stenosis. Spinal stenosis may cause pain, weakness, and numbness on the buttocks, hips, and thighs. It’s frequently associated with other health issues which could lead to facet arthropathy. The natural aging process is frequently considered to be one of the most common indirect sources of facet arthropathy. Other health issues which can ultimately affect the facet joints and cause facet arthropathy include:
- Osteoarthritis: Degeneration of joint cartilage and underlying bone, generally during middle age
- Facet joint degeneration: Wear and tear on the facet joint brought on over time due to aging
- Facet joint injury: Trauma to the facet joints caused by an impact, such as a fall or automobile accident
- Synovial cyst: A fluid-filled sac which develops in the spine, generally as a result of aging
Ischiofemoral Impingement
Ischiofemoral impingement syndrome is a condition which occurs when the ischium and the head of the femur experience excessive amounts of pressure, generally due to trauma, overuse, or surgery. The trauma, overuse, or surgery, can also cause bone spurs to grow along the ischium. This gives the bones an abnormal shape which makes them no longer fit together.
Because these don’t fit properly together anymore, the bones may then start to rub against each other during movement causing friction which can damage the joint and cause painful symptoms. As friction worsens, the pain may also increase and restrict movements. The symptoms for ischiofemoral impingement may vary and treatment can also depend on symptoms.
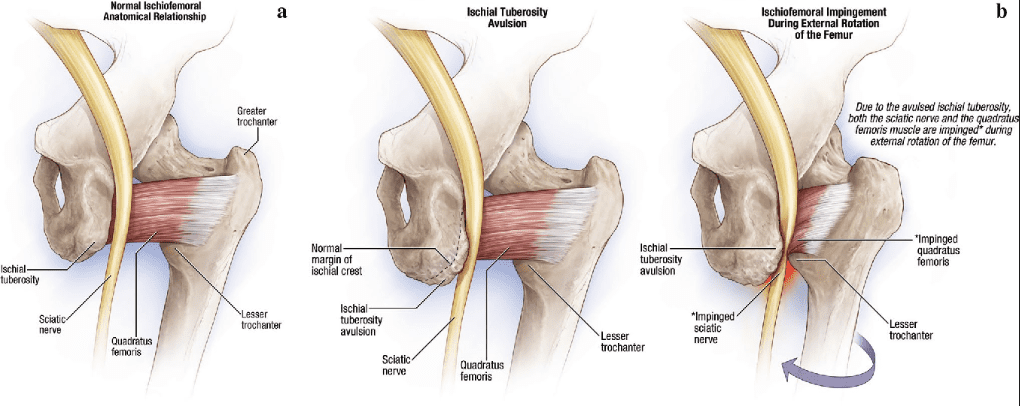
The main symptom of ischiofemoral impingement syndrome is hip pain. The pain from this underlying health issue may start off as mild, however, it can often worsen as the rubbing of the bones causes more damage and inflammation. Ischiofemoral impingement syndrome can feel similar to a pulled hamstring but the pain is generally closer to the buttocks like sciatica.
Ischiofemoral impingement occurs due to excess friction between the top of the thighbone, or the femur, and the hip bone, or the ischium. These two bones generally touch in a way which allows them to move without causing pain, however, trauma, overuse, and surgery can ultimately damage the bone. Moreover, if the damage causes a bone spur to grow on the hip or femur, as described above, the extra piece of bone can cause more damage and make the condition worse.
When you seek medical attention for a medical concern, it’s fundamental for the healthcare professional to accurately diagnose your health issue in order to follow-up with the proper treatment. A differential diagnosis is a list of possible injuries and/or underlying conditions which may be causing symptoms. Sciatica, a collection of symptoms commonly characterized by pain, discomfort, tingling sensations, and numbness, is a well-known health issue which can have many differential diagnosis. – Dr. Alex Jimenez D.C., C.C.S.T. Insight
Fibromyalgia Magazine
The purpose of the article was to discuss the differential diagnosis in sciatica with a variety of other health issues. Accurate diagnosis and proper treatment are important for sciatic nerve pain management. The scope of our information is limited to chiropractic, musculoskeletal and nervous health issues as well as functional medicine articles, topics, and discussions. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
Additional Topic Discussion: Severe Sciatica
Back pain is one of the most prevalent causes of disability and missed days at work worldwide. Back pain attributes to the second most common reason for doctor office visits, outnumbered only by upper-respiratory infections. Approximately 80 percent of the population will experience back pain at least once throughout their life. Your spine is a complex structure made up of bones, joints, ligaments, and muscles, among other soft tissues. Injuries and/or aggravated conditions, such as herniated discs, can eventually lead to symptoms of sciatica, or sciatic nerve pain. Sports injuries or automobile accident injuries are often the most frequent cause of painful symptoms, however, sometimes the simplest of movements can have these results. Fortunately, alternative treatment options, such as chiropractic care, can help ease sciatic nerve pain, or sciatica, through the utilization of spinal adjustments and manual manipulations, ultimately improving pain relief.
Formulas for Methylation Support
XYMOGEN’s Exclusive Professional Formulas are available through select licensed health care professionals. The internet sale and discounting of XYMOGEN formulas are strictly prohibited.
Proudly, Dr. Alexander Jimenez makes XYMOGEN formulas available only to patients under our care.
Please call our office in order for us to assign a doctor consultation for immediate access.
If you are a patient of Injury Medical & Chiropractic Clinic, you may inquire about XYMOGEN by calling 915-850-0900.
For your convenience and review of the XYMOGEN products please review the following link.*XYMOGEN-Catalog-Download
* All of the above XYMOGEN policies remain strictly in force.
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Differential Diagnosis in Sciatica Part 1" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics