Sports Head Injuries: From Concussions to Skull Fractures — What to Know and How Integrative Care Helps

Introduction
Head injuries in sports range from mild to life-threatening. Concussions occur more often than any other head injury in athletics, but more severe problems—like brain contusions, intracranial hematomas, and skull fractures—can also happen. A head impact, whiplash, or a hard jolt can cause the brain to move inside the skull and result in damage. In many cases, chiropractors and integrative medicine teams work alongside medical doctors to help people reduce symptoms, protect the neck and spine, restore balance and vision-related function, and support the body’s natural healing process (Mayo Clinic, n.d.; Cleveland Clinic, n.d.; OrthoInfo/AAOS, n.d.; Carr Chiropractic Clinic, n.d.; ThinkVida, n.d.).
This article explains the types of sports-related head injuries, how to recognize them, why immediate evaluation is crucial, and what a safe recovery plan entails. It also demonstrates how an integrative team, including a chiropractor, can support care when coordinated with primary care, sports medicine, neurology, or emergency services.
Fast facts
-
The most common sports head injury is a concussion, a mild traumatic brain injury (mTBI) caused by a blow to the head or body that makes the head move quickly (Cleveland Clinic, n.d.; OrthoInfo/AAOS, n.d.).
-
More severe injuries include brain contusions, epidural or subdural hematomas, and skull fractures, which may require emergency treatment (Adelson et al., 2014; Marcolini & Keegan, 2020; Children’s Minnesota, n.d.; Mayo Clinic, n.d.).
-
Sports with higher concussion rates include football, ice hockey, wrestling, soccer, and basketball, though concussions can occur in many activities—even non-contact sports (CDC, n.d.; Neural Effects, n.d.; Arsenian Law Firm, n.d.).
-
Symptoms may be immediate or delayed and can include headache, dizziness, nausea, fogginess, sensitivity to light and noise, balance issues, and neck pain. Loss of consciousness is not required (Cleveland Clinic, n.d.; Mayo Clinic, n.d.).
-
A stepwise, graded return-to-play approach helps athletes recover safely after a concussion (McCrory et al., 2013; OrthoInfo/AAOS, n.d.).
What counts as a sports head injury?
Concussion (mild traumatic brain injury)
A concussion happens when the brain moves quickly inside the skull due to a hit, fall, or sudden shake. This movement stretches and disrupts brain cells, potentially altering the way the brain functions for a short time. Common symptoms include headache, dizziness, feeling “off,” balance problems, slowed thinking, or trouble concentrating (Cleveland Clinic, n.d.; Mayo Clinic, n.d.; WebMD, n.d.).
Key point: You do not need to be knocked out to have a concussion. Symptoms can start immediately or occur hours later (Cleveland Clinic, n.d.; Mayo Clinic, n.d.).
Brain contusion
A contusion is a bruise to the brain tissue from a direct blow. It can occur with or without a skull fracture. Depending on size and location, it may cause confusion, drowsiness, weakness, or seizures and can be dangerous if swelling develops (Adelson et al., 2014; Marcolini & Keegan, 2020).
Intracranial hematomas (epidural and subdural)
-
Epidural hematoma (EDH): Bleeding between the skull and the dura (the outer brain covering), often from an artery. Sometimes, there is a “lucid interval” followed by a rapid decline—this is considered an emergency (Marcolini & Keegan, 2020).
-
Acute subdural hematoma (SDH): Bleeding beneath the dura, often from torn bridging veins. SDH can progress quickly and is linked with high risk when severe (Marcolini & Keegan, 2020).
These injuries may require urgent neurosurgical care. Any athlete with red-flag signs should be sent to the emergency department immediately.
Skull fractures
A skull fracture is a break in the skull bone caused by significant force. Signs can include swelling, bruising behind the ears or around the eyes, clear fluid from the nose or ears, or a depressed skull area. These injuries often require imaging and close medical monitoring (Children’s Minnesota, n.d.; WebMD, n.d.).
How do these injuries happen?
Most sports head injuries come from a direct blow to the head or from a forceful body impact that rapidly moves the head and neck (Cleveland Clinic, n.d.; OrthoInfo/AAOS, n.d.). Collisions, takedowns, checking, falls, heading a ball, or accidental hits from equipment can all be triggers (CDC, n.d.; Arsenian Law Firm, n.d.; Aptiva Health, n.d.). Even in sports viewed as “non-contact,” an awkward fall or impact can still cause a concussion (Arsenian Law Firm, n.d.).
Neck mechanics matter. When the neck cannot brace effectively—due to weak muscles or poor alignment—the head may accelerate more during impact, increasing strain on the brain and the upper cervical spine (Carr Chiropractic Clinic, n.d.; Aurora Chiropractic, n.d.; Mountain Movement Center, n.d.).
Who is most at risk?
All athletes, including youth and adults, can be at risk. U.S. surveillance shows high concussion rates in football, ice hockey, wrestling, soccer, and basketball. Many concussions in basketball happen during player collisions, not just falls (CDC, n.d.). Youth and high-school settings see a large share of sports-related concussions due to participation volume and developmental factors (Neural Effects, n.d.). Wrestling and martial arts involve throws and takedowns; soccer involves heading and collisions; cycling and skating involve falls at speed (CDC, n.d.; Arsenian Law Firm, n.d.; Aptiva Health, n.d.; GSA Medicine, n.d.).
Signs and symptoms: When to act now
Common concussion symptoms
Headache, pressure in the head, dizziness, nausea or vomiting, balance problems, sensitivity to light or noise, feeling foggy or slowed, trouble concentrating or remembering, sleep issues, and mood changes (Cleveland Clinic, n.d.; OrthoInfo/AAOS, n.d.; WebMD, n.d.).
Red-flag signs—call emergency services immediately
Worsening headache, repeated vomiting, unequal pupils, weakness or numbness, slurred speech, seizure, increasing confusion, unusual drowsiness, loss of consciousness, or symptoms that quickly get worse (Mayo Clinic, n.d.; Cleveland Clinic, n.d.; OrthoInfo/AAOS, n.d.).
Headache triggers in sports
Lifting heavy weights or engaging in high-pressure activities can sometimes trigger or worsen headaches in individuals prone to them (Studio Athletica, n.d.). New or severe headache after a head or neck injury should be medically evaluated (Cleveland Clinic, n.d.; OrthoInfo/AAOS, n.d.).
Evaluation and diagnosis
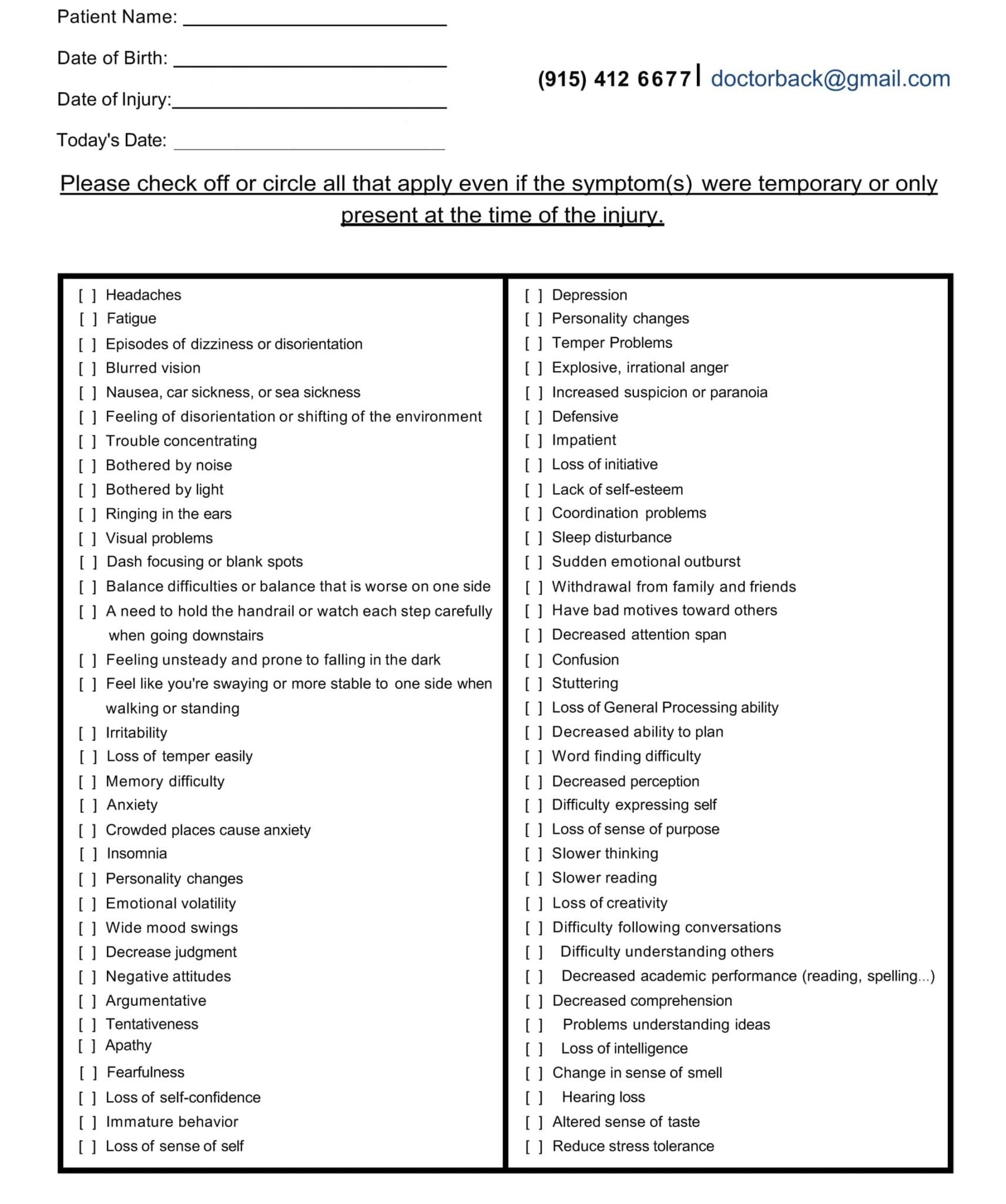
A trained clinician gathers a history of the hit or whiplash event, reviews symptoms, and performs a focused neurologic exam. They may use symptom checklists, balance and eye movement tests, and memory screens specifically designed for concussion evaluation. Imaging (CT or MRI) is usually reserved for suspected bleeding, skull fracture, or other serious findings (OrthoInfo/AAOS, n.d.; Mayo Clinic, n.d.; Cleveland Clinic, n.d.).
For suspected epidural or subdural hematoma, skull fracture, persistent vomiting, seizure, focal weakness, or rapidly worsening symptoms, urgent imaging and emergency referral are standard (Marcolini & Keegan, 2020; Children’s Minnesota, n.d.; Mayo Clinic, n.d.).
Initial management
-
Remove from play right away. Do not return the same day if concussion is suspected (OrthoInfo/AAOS, n.d.).
-
Rest briefly, then gradually reintroduce activity. Relative rest for 24–48 hours (light daily activity) is typical, followed by a stepwise increase in cognitive and physical activity as tolerated (McCrory et al., 2013; OrthoInfo/AAOS, n.d.; Mayo Clinic, n.d.).
-
Monitor symptoms and sleep. Avoid risky activities that could cause another head injury.
-
Follow medical guidance for school/work accommodations and sports progression (OrthoInfo/AAOS, n.d.).
The graded return-to-play path (6-stage concept)
A well-known approach uses a 6-stage progression. Each stage lasts at least 24 hours. If symptoms return, drop back to the previous step:
-
Symptom-limited activity (light daily tasks)
-
Light aerobic exercise (e.g., walking or light cycling)
-
Sport-specific exercise (no head impact)
-
Non-contact training drills (progressive resistance)
-
Full-contact practice (after medical clearance)
-
Return to competition
If symptoms worsen at any stage, rest and return to the previous step until stable (McCrory et al., 2013; OrthoInfo/AAOS, n.d.; Alla et al., 2012).
Integrative care: How chiropractors fit into the team
Chiropractors do not diagnose or treat bleeding inside the skull, skull fractures, or other emergencies. Those require immediate medical care. However, within a coordinated care plan, a chiropractor trained in sports and concussion-sensitive care may help with:
-
Neck and upper back mechanics
Gentle, patient-specific techniques to address cervical and thoracic joint dysfunction, muscle tension, and posture after injury—always timed and titrated to symptoms and medical guidance (Aurora Chiropractic, n.d.; Carr Chiropractic Clinic, n.d.; Mountain Movement Center, n.d.). -
Vestibular and oculomotor rehab support
In collaboration with physical therapists or neuro-rehab specialists, targeted exercises can improve balance, gaze stability, and motion sensitivity that often follow a concussion (OrthoInfo/AAOS, n.d.; McCrory et al., 2013). -
Headache and neck pain strategies
Soft-tissue work, gentle mobilization, and home exercises for the cervical spine may help reduce cervicogenic contributions to post-concussion headaches, when medically appropriate (Studio Athletica, n.d.; Carr Chiropractic Clinic, n.d.; Mountain Movement Center, n.d.). -
Graded exercise guidance
Under the medical plan, clinicians may help athletes progress through light aerobic work, strength training, and sport-specific drills while tracking symptom response (OrthoInfo/AAOS, n.d.; McCrory et al., 2013). -
Education and coordination
Chiropractors coordinate with MDs/DOs, NPs, PTs, athletic trainers, and neuro-specialists for imaging decisions, medication needs, school/work notes, and clearance timing (Carr Chiropractic Clinic, n.d.; ThinkVida, n.d.).
Clinical note (Dr. Alexander Jimenez, DC, APRN, FNP-BC): In a dual-scope, integrative clinic, we often see persistent neck stiffness, suboccipital tightness, and balance problems after concussions—especially when the initial impact involved a whiplash component. A careful, team-based plan—starting with medical screening and emergency rule-outs—then layering in graded activity, cervical stabilization, vestibular/oculomotor exercises, and posture work tends to yield steady progress. Consistent communication with the athlete’s primary provider and athletic training staff is key for safe return-to-play (Jimenez, n.d.-a; Jimenez, n.d.-b).
What recovery can look like
Early phase (first 24–48 hours): Relative rest, symptom monitoring, hydration, regular sleep, and light cognitive activity as tolerated (Mayo Clinic, n.d.; OrthoInfo/AAOS, n.d.).
Subacute phase: Gradual return to school/work with short breaks; light aerobic activity; targeted neck and balance drills if cleared; attention to visual triggers (screen brightness, busy environments) (McCrory et al., 2013; OrthoInfo/AAOS, n.d.).
Later phase: Progressive resistance training, sport-specific movements, and non-contact practice; continued neck mobility/stability work; final clearance for full contact and competition once symptom-free and medically approved (McCrory et al., 2013; OrthoInfo/AAOS, n.d.).
Complicated courses: Headaches that worsen, repeated vomiting, increasing confusion, focal deficits, or seizures require urgent medical evaluation (Mayo Clinic, n.d.; Cleveland Clinic, n.d.). Post-concussion symptoms that last beyond typical recovery windows may benefit from referrals (neurology, vision therapy, vestibular PT, mental health) (OrthoInfo/AAOS, n.d.; Cleveland Clinic, n.d.).
Prevention tips that actually help
-
Technique and rules: Teach proper tackling, checking, and falling techniques; follow rules that reduce dangerous contact (CDC, n.d.; OrthoInfo/AAOS, n.d.).
-
Protective gear: Sport-appropriate helmets and mouthguards (while helmets do not “prevent” concussion, they reduce certain head and face injuries). Fit and condition matter (OrthoInfo/AAOS, n.d.).
-
Neck strength and posture: Conditioning programs that improve cervical strength and dynamic posture may help reduce head acceleration during impacts (Carr Chiropractic Clinic, n.d.; Mountain Movement Center, n.d.).
-
Culture of safety: Encourage honest symptom reporting, quick removal from play, and team-wide respect for recovery timelines (CDC, n.d.; OrthoInfo/AAOS, n.d.).
Special focus: Subdural vs. epidural hematoma
Acute subdural hematoma (SDH) often results from tearing of bridging veins and can progress quickly. Symptoms may include severe headache, drowsiness, weakness, or confusion. This is a medical emergency and may require neurosurgery (Marcolini & Keegan, 2020).
Epidural hematoma (EDH) can follow a skull fracture with arterial bleeding. Some people may appear “okay” at first and then worsen fast. This is also a medical emergency (Marcolini & Keegan, 2020).
Bottom line: Any red flags after a head or neck impact need immediate emergency care.
When to seek care and who to see
-
Emergency care now: If red-flag signs are present (seizure, repeated vomiting, severe headache that worsens, slurred speech, weakness/numbness, unequal pupils, confusion that worsens, or unusual drowsiness) (Mayo Clinic, n.d.; Cleveland Clinic, n.d.).
-
Primary care/sports medicine/neurology: For evaluation, imaging decisions, and school/work/sport guidance (OrthoInfo/AAOS, n.d.).
-
Chiropractic and integrative team: To support neck mechanics, balance/oculomotor rehab collaboration, graded exercise, and symptom-guided progress—only after emergency issues are ruled out and in coordination with the lead medical provider (Carr Chiropractic Clinic, n.d.; ThinkVida, n.d.; Mountain Movement Center, n.d.; Aurora Chiropractic, n.d.).
Practical recovery checklist (athletes & families)
-
Stop play if a concussion is suspected.
-
Clinical assessment on the same day.
-
Rest briefly (24–48 hours), then gradual activity as tolerated.
-
Follow a 6-stage return-to-play plan.
-
Communicate with coaches, trainers, and clinicians.
-
Address the neck and posture with safe, guided care after medical clearance.
-
Prioritize sleep, hydration, and a balanced diet.
-
Seek urgent care if any red flags appear.
Conclusion
Concussions are the most common sports head injury, but more serious problems—like epidural or subdural hematomas, brain contusions, and skull fractures—also occur. Quick recognition, same-day removal from play, medical evaluation, and a graded return-to-activity plan protect the brain and the athlete’s future. Within a coordinated, physician-led plan, chiropractic and integrative care can help address neck mechanics, headache triggers, balance and vision-related issues, and overall conditioning, enabling athletes to return safely and confidently. Teamwork delivers the best outcome.
References
Adelson, P. D., Bratton, S. L., Carney, N. A., Chesnut, R. M., du Coudray, H. E., et al. (2014). Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents (update of 2003; originally 2003, updated 2012). https://pmc.ncbi.nlm.nih.gov/articles/PMC3959977/
Alla, S., Sullivan, S. J., McCrory, P., Schneiders, A. G., & Hale, L. (2012). The 6-stage return-to-play progression following sports concussion. https://pmc.ncbi.nlm.nih.gov/articles/PMC3838718/
Aptiva Health. (n.d.). Sports injuries & conditions: Head injuries overview. https://www.aptivahealth.com/sports-injuries-conditions#:~:text=The%20most%20common%20athletic%20head%20injury%20is,long%2Dterm%20problems%20with%20memory%20and%20executive%20function.
Arsenian Law Firm. (n.d.). Most common sports that lead to brain injuries. https://www.arsenian.com/blog/most-common-sports-that-lead-to-brain-injuries/#:~:text=Throws%2C%20slams%2C%20and%20takedowns%20can%20result%20in,is%20generally%20considered%20a%20non%2Dcontact%20sport%2C%20head
Aurora Chiropractic. (n.d.). Chiropractic care for head injuries. https://aurora-chiropractic.com/chiropractic-care-for-head-injuries/#:~:text=Spinal%20manipulation%20adjusts%20the%20spine,discomfort%20after%20a%20head%20injury.
Carr Chiropractic Clinic. (n.d.). The role of chiropractic care in concussion management. https://www.carrchiropracticclinic.com/the-role-of-chiropractic-care-in-concussion-management/#:~:text=1.,Collaboration%20with%20Healthcare%20Teams:
Centers for Disease Control and Prevention (CDC). (n.d.). HEADS UP: Data on sports & recreation-related concussions. https://www.cdc.gov/heads-up/data/index.html#:~:text=Some%20sports%20with%20the%20highest%20rates%20of,school%20basketball%20result%20from%20collisions%20among%20athletes
Children’s Minnesota. (n.d.). Skull fracture. https://www.childrensmn.org/educationmaterials/childrensmn/article/21929/skull-fracture/#:~:text=A%20skull%20fracture%20is%20caused%20by%20a,or%2C%20unfortunately%2C%20in%20circumstances%20of%20child%20abuse.
Cleveland Clinic. (n.d.). Concussion: Symptoms & causes. https://my.clevelandclinic.org/health/diseases/15038-concussion#:~:text=Concussion%20symptoms%20may%20start%20right,(fainting%20or%20passing%20out).
Cleveland Clinic. (n.d.). Head injury overview. https://my.clevelandclinic.org/health/diseases/head-injury#:~:text=Headaches.,Seizures.
GSA Medicine. (n.d.). Common head injuries in athletes: Signs and treatments. https://gsamedicine.com/common-head-injuries-in-athletes-signs-and-treatments/#:~:text=The%20most%20common%20sports%2Drelated,mention%20require%20immediate%20emergency%20care.
Jimenez, A. (n.d.-a). Clinical insights on concussion and integrative care. https://dralexjimenez.com/
Jimenez, A. (n.d.-b). Professional profile and clinical updates. https://www.linkedin.com/in/dralexjimenez/
Marcolini, E. G., & Keegan, J. (2020). Traumatic brain injury: Subdural hematomas and emergency considerations. https://pmc.ncbi.nlm.nih.gov/articles/PMC7755598/#:~:text=Acute%20subdural%20hematoma%20(SDH)%20is%20the%20most,of%20bridging%20veins%20crossing%20the%20subdural%20space.
Mayo Clinic. (n.d.). Concussion: Symptoms & causes. https://www.mayoclinic.org/diseases-conditions/concussion/symptoms-causes/syc-20355594#:~:text=clues%20may%20include:-,Dazed%20appearance.,Seizures%20or%20convulsions.
Mayo Clinic. (n.d.). Traumatic brain injury: Diagnosis & treatment. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/diagnosis-treatment/drc-20378561#:~:text=Mild%20injury,return%20to%20normal%20routines%20gradually.
McCrory, P., Meeuwisse, W., Aubry, M., Cantu, R., Dvorak, J., et al. (2013). Consensus statement on concussion in sport (Zurich 2012). https://pmc.ncbi.nlm.nih.gov/articles/PMC3838718/
Mountain Movement Center. (n.d.). Addressing sports injuries with chiropractic (concussions & mechanics). https://www.mountainmovementcenter.com/post/addressing-common-sports-injuries-with-chiropractic#:~:text=Concussions,focus%2C%20balance%2C%20and%20coordination.
Neural Effects. (n.d.). Do high-school sports cause most concussions? https://neuraleffects.com/blog/high-school-sports-cause-most-concussions/
OrthoInfo—American Academy of Orthopaedic Surgeons (AAOS). (n.d.). Sports concussion: Diagnosis, management, and return to play. https://orthoinfo.aaos.org/en/diseases–conditions/sports-concussion/#:~:text=of%20concussion%20include:-,Drowsiness,doctor%20will%20order%20imaging%20scans.
Studio Athletica. (n.d.). Headaches in athletes and triggers (including lifting). https://www.studioathletica.com/conditions-treatments/spine-physiotherapy/headache/#:~:text=Headaches%2C%20a%20pain%20that%20can%20affect%20the,increase%20in%20blood%20pressure%2C%20such%20as%20weightlifting.
ThinkVida. (n.d.). Treating concussions with chiropractic care (team-based approach). https://thinkvida.com/blog/treating-concussions-with-chiropractic-care/
WebMD. (n.d.). Head injuries: Causes & treatments. https://www.webmd.com/fitness-exercise/head-injuries-causes-and-treatments
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Chiropractic for Sports Head Injuries Treatment Options" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



