Can Head Injuries Lead to Sciatica? An Easy Guide to What Happens and How Integrative Chiropractic Care May Help

Key idea: Head injuries do not only affect the brain. They can also change how muscles in the neck, back, and hips work. Those changes can irritate or compress the sciatic nerve, making sciatica more likely or more severe. In some cases, trauma can even trigger abnormal bone growth around soft tissues (heterotopic ossification) that narrows the space around nerves and limits motion. Integrative chiropractic care, when coordinated with medical providers, may help reduce pain, restore better movement, and support healing after a head injury.
What Is Sciatica?
Sciatica is pain, tingling, burning, or numbness that travels from the lower back or buttocks down the back of one leg. It happens when the sciatic nerve is irritated or compressed. The cause may be a bulging or herniated disc, spinal stenosis, piriformis muscle tension, post-surgical scar tissue, or post-traumatic soft-tissue changes. Sciatica can feel sharp or electric. It can flare when you sit, cough, sneeze, or bend forward. In severe cases, it can cause the leg to weaken (Arrowhead Clinic, n.d.).
How Can a Head Injury Trigger or Worsen Sciatica?
Brain control of spinal muscles can “misfire” after a concussion or TBI
The brain controls postural muscles throughout the spine. After a concussion or traumatic brain injury (TBI), the brain’s ability to coordinate muscle tone and timing can be disrupted. This can cause protective muscle guarding, loss of normal activation in the core and glute muscles, or asymmetry from left to right. Over time, this “motor control drift” can pull the pelvis and lumbar segments out of their usual alignment and irritate the sciatic nerve (Broadview Health Centre, n.d.; Physio Pretoria, n.d.; Reis, n.d.). Clinical studies also show that pain after TBI is common and influenced by neurological and inflammatory factors (Nampiaparampil et al., n.d.; Science Reports, n.d.).
Why this matters: If deep stabilizers (such as the multifidus and transverse abdominis) stop firing properly, larger surface muscles take over. This can compress joints, strain discs, and tighten piriformis or hamstring tissues. Any of these can increase nerve irritation and produce sciatic pain (Arrowhead Clinic, n.d.; Dr. Kal, n.d.).
Upper cervical misalignment can cascade down the chain
Severe head and brain injuries may disrupt the position of the upper cervical spine (C0–C2). When the top of the neck loses its normal balance, the head shifts slightly to compensate. The body compensates through the lower neck, upper back, and pelvis. This creates uneven loading through the sacroiliac joints and the lumbar spine, where the sciatic nerve roots exit. That “top-down” chain can increase pressure on the sciatic nerve and trigger pain down one leg (Broadview Health Centre, n.d.; Physio Pretoria, n.d.; OK Precision Chiropractic, n.d.). Clinically, chiropractors often see upper-cervical dysfunction after concussion, whiplash, or falls—patterns that can contribute to persistent low-back and leg symptoms.
Head injuries raise the risk of other spine injuries
Research shows that patients with head trauma have a higher risk of having spinal injuries at the same time (co-injuries), especially with significant mechanisms like falls or motor vehicle crashes (Hicks et al., n.d.). That means the sciatica may not only come from altered muscle control, but also from a true disc injury, facet injury, or sacroiliac joint trauma that happened with the head injury (Hicks et al., n.d.; Arrowhead Clinic, n.d.).
Inflammation and nervous-system sensitization after TBI
After a TBI, inflammatory signaling can persist and increase pain sensitivity. Animal and human data suggest that certain chemokine pathways (for example, those acting at CXCR2) can amplify pain behaviors after brain injury (Science Reports, n.d.). Clinical studies also note that chronic pain is common after TBI and is shaped by both biomedical and psychosocial factors (Nampiaparampil et al., n.d.). This primed, sensitive system can “overreact” to mechanical inputs from the lumbar spine or hip, so a mild pinch on the sciatic nerve might feel much worse (Nampiaparampil et al., n.d.; Broadview Health Centre, n.d.).
Heterotopic ossification (HO) can narrow the soft-tissue space around nerves
After trauma, the body can form extra bone in soft tissues, a condition known as heterotopic ossification (HO). HO occurs in some patients with TBI and can limit joint motion, compress nearby tissues, and complicate rehabilitation (Genet et al., n.d.; Potter et al., n.d.). When HO develops around the hip or along the course of the sciatic nerve, it can reduce the space available for the nerve to glide, increasing sciatica-like symptoms and stiffness (Genet et al., n.d.). Early recognition is crucial because HO can progress over time, and “pseudocapsule” scarring may complicate later care (Potter et al., n.d.).
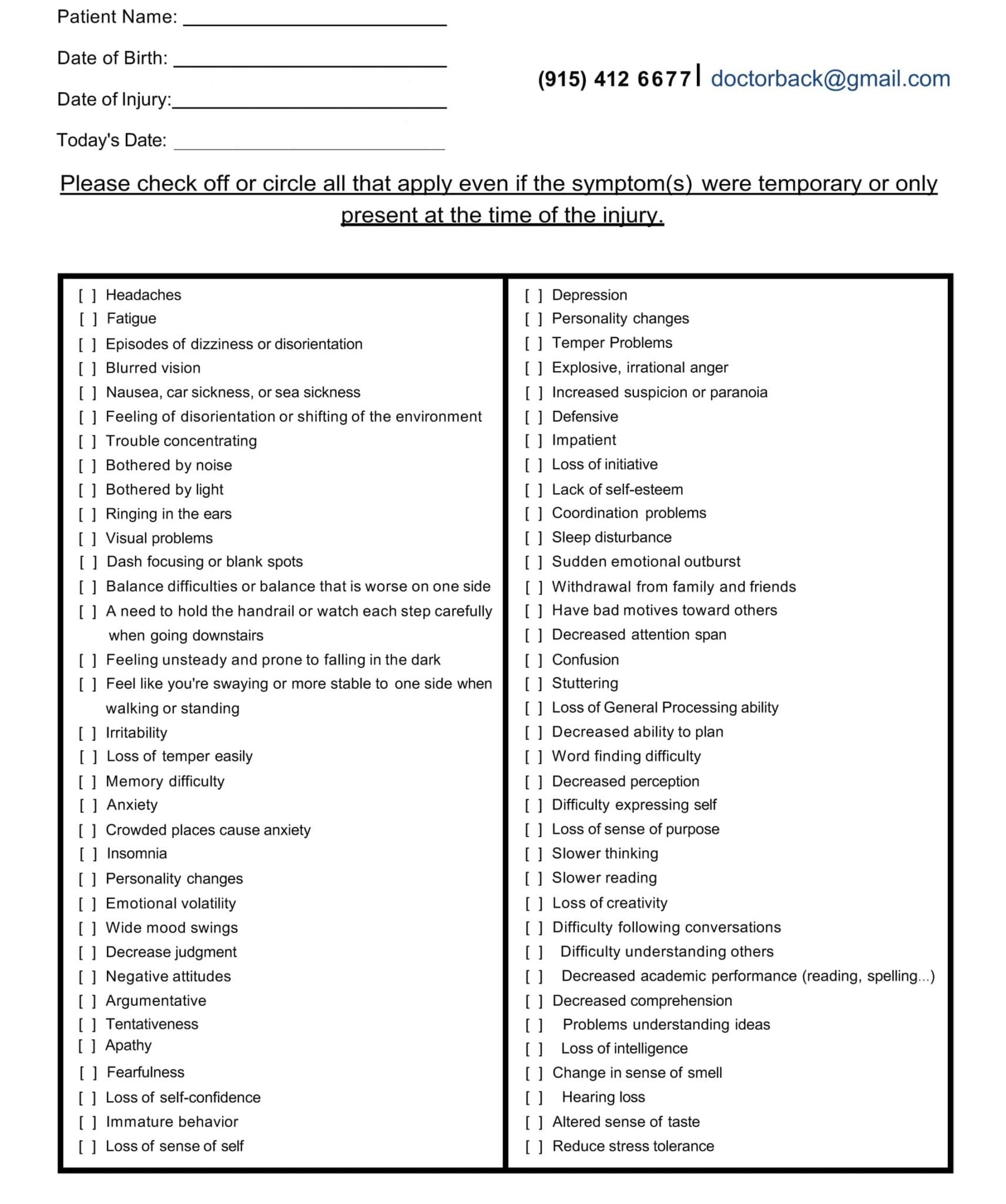
Head Injury/TBI Symptom Questionnaire:
The “Head–Neck–Back–Hip” Chain: A Simple Picture
-
Head injury → brain processing changes, neck strain, or both.
-
Upper cervical shift → downstream compensations in mid-back and pelvis.
-
Pelvic rotation or lumbar guarding → nerve root irritation and sciatic pain.
-
Inflammation and sensitization after TBI → pain feels stronger and lasts longer.
-
Possible HO near the hip or sciatic path → more mechanical pressure and stiffness.
(Broadview Health Centre, n.d.; Physio Pretoria, n.d.; OK Precision Chiropractic, n.d.; Genet et al., n.d.; Potter et al., n.d.; Science Reports, n.d.; Nampiaparampil et al., n.d.; Arrowhead Clinic, n.d.)
Signs You Might Notice After a Head Injury
-
New or worse low-back or buttock pain radiating down one leg
-
Hip stiffness or a deep ache that limits sitting, squatting, or walking
-
Neck pain, headaches, dizziness, or visual strain that flare with screens or quick head turns (Broadview Health Centre, n.d.; Physio Pretoria, n.d.)
-
Muscle fatigue in the core and glutes; the leg feels “weak”
-
Pain sensitivity that seems “out of proportion” (Nampiaparampil et al., n.d.)
-
A feeling that your posture is crooked or your foot “toes-out” on one side
-
Trouble tolerating long car rides or standing in line (Arrowhead Clinic, n.d.)
Red flags: New bowel or bladder loss, true foot drop, rapidly worsening weakness, fever, unexplained weight loss, or severe, unrelenting night pain. Seek urgent medical evaluation.
How Integrative Chiropractic Care Fits In
Integrative chiropractic care combines spinal assessment and gentle adjustments with soft-tissue therapy, exercise progressions, balance/vestibular retraining, and lifestyle support. In complex TBI-related cases, chiropractors often work closely with primary care, neurology, physiatry, and physical therapy.
A careful assessment comes first
-
History: injury details, concussion symptoms, neck pain, visual strain, dizziness, sleep, and cognitive load (Reis, n.d.; Pinnacle Health Chiropractic, n.d.; Addison Sports Clinic, n.d.).
-
Screening: red flags, co-injuries (Hicks et al., n.d.), and HO risk factors (Genet et al., n.d.; Potter et al., n.d.).
-
Exam: upper cervical alignment, cervicogenic dizziness signs, rib cage motion, sacroiliac joint irritation, piriformis tension, hip rotation limits, neural tension tests, and gait.
-
Imaging: Guided by findings—when indicated, MRI or CT for structural concerns; ultrasound can aid in monitoring soft tissue around the hip.
Gentle spinal and pelvic realignment
Upper cervical and lumbopelvic adjustments aim to restore better joint motion and reduce asymmetrical loading that irritates the sciatic nerve. Techniques are matched to tolerance—often low-force methods early on (Zaker Chiropractic, n.d.; Team Allied, n.d.; Dr. Kal, n.d.; Arrowhead Clinic, n.d.). Improved alignment can reduce strain on nerve roots and relieve muscular guarding.
Soft-tissue care to free the nerve
Myofascial release, instrument-assisted techniques, and targeted stretching for the piriformis, deep hip rotators, and hamstrings can restore nerve glide. This is combined with gentle neural mobilization when appropriate (Arrowhead Clinic, n.d.; Dr. Kal, n.d.).
Core, hip, and balance retraining
Because TBI can disrupt brain-to-muscle communication, rehabilitation focuses on the deep core, including the gluteus medius and maximus, and the hip rotators to stabilize the pelvis. Balance and vestibular exercises help retrain head–eye–body coordination, allowing the lumbar spine to stop overworking (Physio Pretoria, n.d.; Addison Sports Clinic, n.d.; Pinnacle Health Chiropractic, n.d.).
Inflammation modulation and nervous-system calm
Integrative plans support sleep, stress reduction, and a gradual increase in activity. Together, these steps can help reduce neuroinflammation and central sensitization, which amplify pain after TBI (Science Reports, n.d.; Nampiaparampil et al., n.d.). As symptoms subside, patients can perform stronger core and hip exercises without experiencing flare-ups (Pinnacle Health Chiropractic, n.d.).
Cerebrospinal fluid (CSF) flow considerations
Some integrative chiropractic discussions note that improving spinal mechanics and reducing dural tension may support better CSF circulation, which can be altered by serious injuries (Apex Chiropractic, n.d.). While this area requires further research, many clinics incorporate gentle techniques for cranio-cervical mobility, alongside posture and breathing exercises, to reduce strain.
If HO is suspected
When limited hip motion, deep stiffness, and progressive restriction point toward HO, coordinated care is essential. Medical teams confirm the diagnosis, track progression, and guide treatment. Chiropractic care can still support posture, spinal mechanics, and pain control, while the medical plan addresses HO directly (Genet et al., n.d.; Potter et al., n.d.).
A Practical Recovery Roadmap (6 Simple Phases)
-
Settle the system (Weeks 0–2)
-
Relative rest, sleep hygiene, gentle neck/hip mobility, diaphragmatic breathing, and walking as tolerated.
-
Light manual therapy to reduce guarding; screen red flags (Hicks et al., n.d.).
-
Education about pacing and flare management (Nampiaparampil et al., n.d.).
-
-
Re-align and re-activate (Weeks 2–6)
-
Gentle upper-cervical and pelvic adjustments within comfort (Zaker Chiropractic, n.d.).
-
Isometric core/glute activation; short holds, frequent sets.
-
Begin balance drills (head turns, eyes-closed stance as tolerated) (Physio Pretoria, n.d.).
-
-
Restore nerve glide and hip motion (Weeks 4–8)
-
Piriformis/hamstring mobility, sciatic nerve sliders as indicated.
-
Progress to bridges, hip abduction, and controlled step-downs.
-
Graded sitting tolerance; micro-breaks for desk work (Arrowhead Clinic, n.d.; Dr. Kal, n.d.).
-
-
Build capacity (Weeks 6–12)
-
Dead-bug progressions, side planks, and single-leg work.
-
Heavier carries (such as a farmer’s carry or suitcase) to train anti-tilt stability.
-
Longer balance/vestibular sessions; add dual-tasking (Pinnacle Health Chiropractic, n.d.; Addison Sports Clinic, n.d.).
-
-
Return to desired activities (Weeks 8–16)
-
Sport- or job-specific drills with load and speed control.
-
Maintain posture programming to protect the sciatic nerve during long days.
-
-
Maintain and prevent (Ongoing)
-
Short daily mobility, 2–3 strength sessions weekly, and sleep/stress routines for inflammation control (Pinnacle Health Chiropractic, n.d.; Reis, n.d.).
-
Timelines vary. If symptoms worsen or red flags appear, contact your medical team immediately.
Clinical Insights from Dr. Alexander Jimenez, DC, APRN, FNP-BC
In patients recovering from motor vehicle accidents, sports injuries, and falls, Dr. Jimenez’s integrative approach focuses on dual-scope assessment (chiropractic and nurse practitioner perspectives), careful upper cervical evaluation, and lumbopelvic mechanics to reduce sciatic nerve irritation. He emphasizes graded vestibular and balance work to restore head–neck–hip harmony, plus core and glute progressions that reduce strain on the lumbar discs and nerve roots. His team coordinates with imaging and medical specialists when HO or structural co-injuries are suspected and educates patients on pacing, sleep, and inflammation control to maintain steady progress and minimize flares (Jimenez, n.d.-a; Jimenez, n.d.-b).
Everyday Tips to Protect the Sciatic Nerve During TBI Recovery
-
Move gently, often. Short walks and micro-breaks beat long rest.
-
Neutral head and pelvis. Keep screens at eye level. Avoid slouching and chin-poking.
-
Breathe low and slow. Diaphragmatic breathing calms the system and reduces muscle tension, or bracing.
-
Sit smart. Hips slightly above knees; alternate chairs and positions.
-
Load the legs. Simple strength (bridges, sit-to-stand, step-ups) supports the pelvis.
-
Sleep matters. Consistent nights improve pain regulation (Pinnacle Health Chiropractic, n.d.).
-
Work as a team. Blend chiropractic care with medical, therapy, and, when needed, surgical consults.
When to Seek Urgent Help
-
New bowel or bladder loss or numbness in the “saddle” region
-
Fast-worsening weakness, true foot drop, or uncontrolled pain at night
-
Fever or unexplained weight loss
These symptoms need immediate medical evaluation.
Bottom Line
Head injuries can set off changes from the top of the spine to the pelvis. Those changes can disturb posture, tighten or weaken key muscles, and raise inflammation—conditions that can irritate the sciatic nerve. In some cases, trauma can lead to heterotopic ossification that physically narrows soft-tissue spaces near the nerve. An integrative chiropractic plan, coordinated with your medical team, can help realign the spine, restore muscle control, calm the nervous system, and build the strength and balance needed to protect the sciatic nerve during daily activities.
References
-
Addison Sports Clinic. (n.d.). Concussion care. https://addisonsportsclinic.com/concussion-care/#:~:text=Understanding%20the%20Limitations%20of%20Each,such%20as%20anxiety%20and%20depression
-
Apex Chiropractic. (n.d.). How chiropractic care can treat a traumatic brain injury (includes discussion of CSF). https://apexchiroco.com/updates/how-chiropractic-care-can-treat-a-traumatic-brain-injury/#:~:text=Restores%20Cerebrospinal%20Fluid%20Circulation,is%20to%20resolve%20CSF%20circulation
-
Arrowhead Clinic. (n.d.). Chiropractic treatment for sciatica relief: What you need to know. https://www.arrowheadclinic.com/category/blog/chiropractic-treatment-for-sciatica-relief-what-you-need-to-know#:~:text=In%20the%20case%20of%20the,itself%20but%20the%20underlying%20cause
-
Broadview Health Centre. (n.d.). Back pain & concussion connection. https://broadviewhealthcentre.com/back-pain-concussion-connection/#:~:text=A%20potential%20long%2Dterm%20effect,effect%20on%20its%20underlying%20cause
-
Dr. Kal. (n.d.). Chiropractic care for sciatica after an accident. https://drkal.com/chiropractic-care-for-sciatica-after-an-accident/#:~:text=Improving%20Mobility%20with%20Chiropractic%20Techniques,better%20movement%20and%20physical%20ability
-
Genet, F., et al. (n.d.). Heterotopic ossification of the hip following traumatic brain injury. National Center for Biotechnology Information (NCBI). https://pmc.ncbi.nlm.nih.gov/articles/PMC2642541/#:~:text=Capsular%20and%20muscular%20scarring%2C%20hardware,the%20new%20bone%20%5B26%5D
-
Hicks, C. W., et al. (n.d.). Concomitant spine injury in patients with traumatic brain injury. NCBI. https://pmc.ncbi.nlm.nih.gov/articles/PMC3177586/#:~:text=severe%20intracranial%20hematomas.-,Conclusion,risk%20for%20concomitant%20spine%20injury
-
Jimenez, A. (n.d.-a). Clinical observations and integrative care insights. https://dralexjimenez.com/
-
Jimenez, A. (n.d.-b). Professional profile and clinical highlights. https://www.linkedin.com/in/dralexjimenez/
-
Nampiaparampil, D. E., et al. (n.d.). Pain after traumatic brain injury: prevalence and predictors. NCBI. https://pmc.ncbi.nlm.nih.gov/articles/PMC4931745/#:~:text=A%20hierarchical%20linear%20regression%20analysis,associated%20with%20pain%20after%20TBI
-
OK Precision Chiropractic. (n.d.). Concussions and lower back pain. https://www.okprecisionchiro.com/concussions-and-lower-back-pain/#:~:text=Concussions%20Can%20Cause%20Back%20Pain,pain%20in%20the%20lower%20back
-
Pinnacle Health Chiropractic. (n.d.). Six ways chiropractic care supports healing after TBI. https://www.pinnaclehealthchiro.com/blog/six-ways-chiropractic-care-supports-healing-after-tbi#:~:text=Lifestyle%20factors%20play%20a%20significant,regulates%20cognition%20and%20mental%20clarity
-
Physio Pretoria. (n.d.). Neck and concussion—how inflammation changes processing. https://physiopretoria.co.za/pain/neck/concussion#:~:text=The%20inflammation%20reaction,to%20interpret%20and%20process%20information
-
Potter, B. K., et al. (n.d.). Heterotopic ossification after trauma: risks and surgical considerations. PubMed. https://pubmed.ncbi.nlm.nih.gov/18158431/#:~:text=Abstract,an%20upper%2Dmotor%20nerve%20injury.
-
Reis, S. (n.d.). Chiropractic & traumatic brain injuries (WAD and TBI). Northwestern Health Sciences University News. https://www.nwhealth.edu/news/reis-writes-for-chiropractic-economics-chiropractic-and-traumatic-brain-injuries/#:~:text=WAD%20and%20TBI,and%20risks%20for%20future%20injuries
-
Science Reports. (n.d.). Chemokine signaling (CXCR2) and post-TBI pain. Nature. https://www.nature.com/articles/s41598-019-55739-x#:~:text=The%20CXCR2%20receptors%20targeted%20by,the%20pain%20experience%20after%20TBI
-
Team Allied. (n.d.). Chiropractic care for post-concussion syndrome. https://teamalliedpw.com/chiropractic-care-post-concussion-syndrome/#:~:text=If%20you%20play%20intense%20contact,the%20ideal%20choice%20for%20you
-
Zaker Chiropractic. (n.d.). Chiropractic care & head injury rehabilitation. https://zakerchiropractic.com/chiropractic-care-head-injury-rehabilitation/#:~:text=While%20most%20people%20start%20feeling,and%20facilitate%20more%20rapid%20healing
-
Additional resource provided by the user: El Paso Chiropractic—TBI blog category. https://elpasochiropractic.com/f/chiropractic-care-in-el-paso-unlocking-the-secrets-to-recovery?blogcategory=Traumatic+Brain+Injury+%28TBI%29
-
Video reference: Concussion and related topics (YouTube). https://www.youtube.com/watch?v=iBzwl9h5BUw&t=606
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Can Head Injuries Lead to Sciatica Symptoms?" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



