These assessment and treatment recommendations represent a synthesis of information derived from personal clinical experience and from the numerous sources which are cited, or are based on the work of researchers, clinicians and therapists who are named (Basmajian 1974, Cailliet 1962, Dvorak & Dvorak 1984, Fryette 1954, Greenman 1989, 1996, Janda 1983, Lewit 1992, 1999, Mennell 1964, Rolf 1977, Williams 1965).
Clinical Application of Neuromuscular Techniques: Upper Trapezius
Lewit (1999) simplifies the need to assess for shortness by stating, ‘The upper trapezius should be treated if tender and taut.’ Since this is an almost universal state in modern life, it seems that everyone requires MET application to this muscle. Lewit also notes that a characteristic mounding of the muscle can often be observed when it is very short, producing the effect of ‘Gothic shoulders’, similar to the architectural supports of a Gothic church tower (see Fig. 2.13).
Assessment for Shortness of Upper Trapezius (13) (Fig. 4.30)
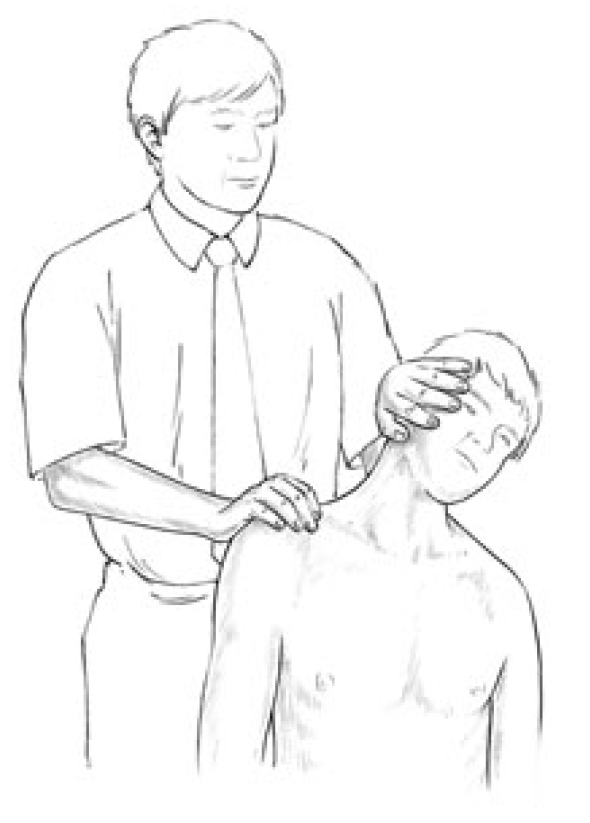
Figure 4.30 Assessment of the relative shortness of the right side upper trapezius. One side is compared with the other (for both the range of unforced motion and the nature of the end-feel of motion) to ascertain the side most in need of MET attention.
Test for upper trapezius for shortness (a) See scapulohumeral rhythm test (Ch. 5) which helps identify excessive activity or inappropriate tone in levator scapula and upper trapezius, which, because they are postural muscles, indicates shortness (Fig 5.13A, B). Greenman (1996) describes a functional ‘firing sequence’ assessment which identifies general imbalance and dysfunction involving the upper and lower fixators of the shoulder (Fig. 4.31).
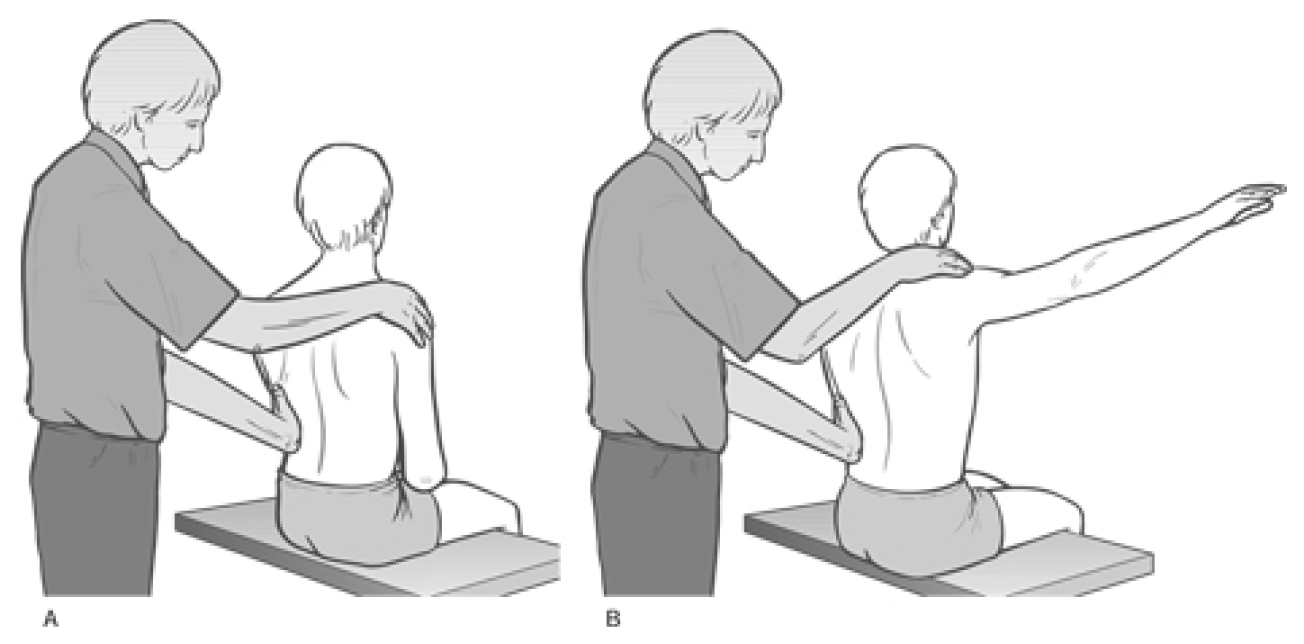
Figure 4.31 Palpation assessment for upper and lower fixators of the shoulder, including upper trapezius (Greenman 1996).
The patient is seated and the practitioner stands behind. The practitioner rests his right hand over the right shoulder area to assess firing sequence of muscles. The other hand can be placed either on the mid-thoracic region, mainly on the side being assessed, or spanning the lower back to palpate quadratus firing. The assessment should be performed at least twice so that various hand positions are used for different muscles (as in Fig. 4.31).
Greenman bases his description on Janda (1983), who notes the ‘correct’ sequence for shoulder abduction, when seated, as involving: supraspinatus, deltoid, infraspinatus, middle and lower trapezius and finally contralateral quadratus. In dysfunctional states the most common substitutions are said to involve: shoulder elevation by levator scapulae and upper trapezius, as well as early firing by quadratus lumborum, ipsilateral and contralateral.
Inappropriate activity of the upper fixators results in shortness, and of the lower fixators in weakness and possible lengthening (see Ch. 2 for discussion of postural/phasic, etc. muscle characteristics).
Test for upper trapezius for shortness (b) The patient is seated and the practitioner stands behind with one hand resting on the shoulder of the side to be tested and stabilising it. The other hand is placed on the ipsilateral side of the head and the head/neck is taken into contralateral sidebending without force while the shoulder is stabilised (see Fig. 4.30).
The same procedure is performed on the other side with the opposite shoulder stabilised. A comparison is made as to which sidebending manoeuvre produced the greater range and whether the neck can easily reach 45° of side-flexion in each direction, which it should. If neither side can achieve this degree of sidebend, then both trapezius muscles may be short. The relative shortness of one, compared with the other, is evaluated.
Test for upper trapezius for shortness (c) The patient is seated and the practitioner stands behind with a hand resting over the muscle on the side to be assessed. The patient is asked to extend the arm at the shoulder joint, bringing the flexed arm/elbow backwards. If the upper trapezius is stressed on that side it will inappropriately activate during this movement. Since it is a postural muscle, shortness in it can then be assumed (see discussion of postural muscle characteristics in Ch. 3).
Test of upper trapezius for shortness (d) The patient is supine with the neck fully (but not forcefully) sidebent contralaterally (away from the side being assessed). The practitioner is standing at the head of the table and uses a cupped hand contact on the ipsilateral shoulder (i.e. on the side being tested) to assess the ease with which it can be depressed (moved caudally) (Fig. 4.32).
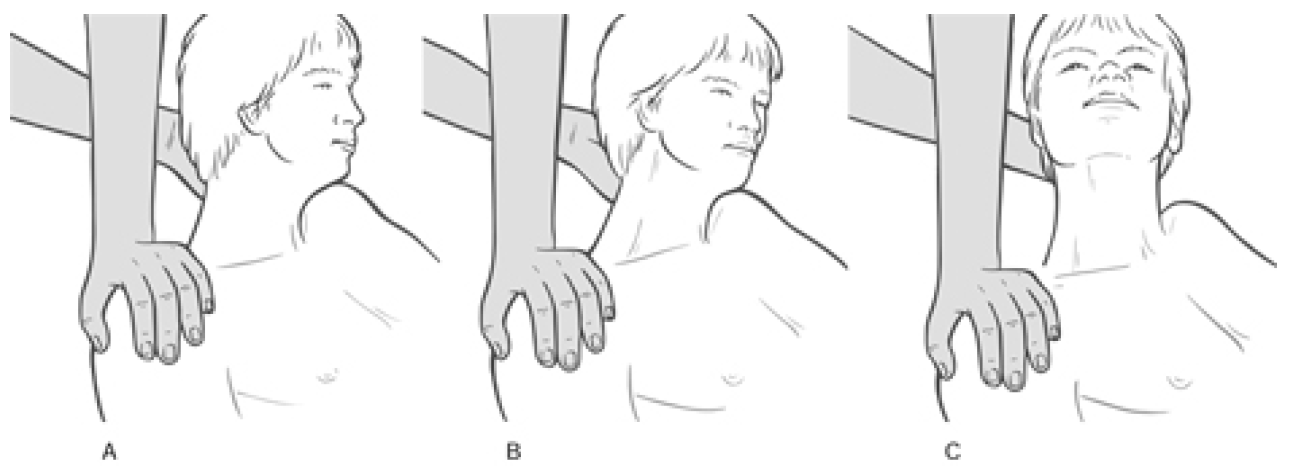
Figure 4.32 MET treatment of right side upper trapezius muscle. A Posterior fibres, B middle fibres, C anterior fibres. Note that stretching in this (or any of the alternative positions which access the middle and posterior fibres) is achieved following the isometric contraction by means of an easing of the shoulder away from the stabilised head, with no force being applied to the neck and head itself.
There should be an easy ‘springing’ sensation as the practitioner pushes the shoulder towards the feet, with a soft end-feel to the movement. If depression of the shoulder is difficult or if there is a harsh, sudden end-point, upper trapezius shortness is confirmed.
This same assessment (always with full lateral flexion) should be performed with the head fully rotated away from the side being treated, half turned away from the side being treated, and slightly turned towards the side being treated, in order to respectively assess the relative shortness and functional efficiency of posterior, middle and anterior subdivisions of the upper portion of trapezius.
MET Treatment of Chronically Shortened Upper Trapezius
MET treatment of upper trapezius, method (a) (Fig. 4.32) In order to treat all the fibres of upper trapezius, MET needs to be applied sequentially. The upper trapezius is subdivided here into anterior, middle and posterior fibres. The neck should be placed into different positions of rotation, coupled with the sidebending as described in the assessment description above, for precise treatment of the various fibres.
The patient lies supine, arm on the side to be treated lying alongside the trunk, head/neck sidebent away from the side being treated to just short of the restriction barrier, while the practitioner stabilises the shoulder with one hand and cups the ear/mastoid area of the same side of the head with the other:
- With the neck fully sidebent and fully rotated contralaterally, the posterior fibres of upper trapezius are involved in the contraction (see below). This will facilitate subsequent stretching of this aspect of the muscle.
- With the neck fully sidebent and half rotated, the middle fibres are involved in the contraction.
- With the neck fully sidebent and slightly rotated towards the side being treated the anterior fibres of upper trapezius are being treated.
The various contractions and subsequent stretches can be performed with practitioner’s arms crossed, hands stabilising the mastoid area and shoulder.
The patient introduces a light resisted effort (20% of available strength) to take the stabilised shoulder towards the ear (a shrug movement) and the ear towards the shoulder. The double movement (or effort towards movement) is important in order to introduce a contraction of the muscle from both ends simultaneously. The degree of effort should be mild and no pain should be felt. The contraction is sustained for 10 seconds (or so) and, upon complete relaxation of effort, the practitioner gently eases the head/neck into an increased degree of sidebending and rotation, where it is stabilised, as the shoulder is stretched caudally.
When stretching is introduced the patient can usefully assist in this phase of the treatment by initiating, on instruction, the stretch of the muscle (‘as you breathe out please slide your hand towards your feet’). This reduces the chances of a stretch reflex being initiated. Once the muscle is being stretched, the patient relaxes and the stretch is held for 10–30 seconds.
CAUTION: No stretch should be introduced from the cranial end of the muscle as this could stress the neck. The head is stabilised at its side-flexion and rotation barrier.
Disagreement
There is some disagreement as to the head/neck rotation position as described in the treatment method above, which calls (for posterior and middle fibres) for sidebending and rotation away from the affected side.
Liebenson (1996), suggests that the patient ‘lies supine with the head supported in anteflexion and laterally flexed away and rotated towards the side of involvement’.
Lewit (1985b) suggests: ‘The patient is supine … the therapist fixes the shoulder from above with one hand, sidebending the head and neck with the other hand so as to take up the slack. He then asks the patient to look towards the side away from which the head is bent, resisting the patient’s automatic tendency to move towards the side of the lesion.’ (This method is described below.)
The author has used the methods described above with good effect and urges readers to try these approaches as well as those of Liebenson and Lewit, and to evaluate results for themselves.
MET treatment of acutely shortened upper trapezius, method (b) Lewit suggests the use of eye movements to facilitate initiation of PIR before stretching, an ideal method for acute problems in this region.
The patient is supine, while the practitioner fixes the shoulder and the sidebent (away from the treated side) head and neck at the restriction barrier and asks the patient to look, with the eyes only (i.e. not to turn the head), towards the side away from which the neck is bent.
This eye movement is maintained, as is a held breath, while the practitioner resists the slight isometric contraction that these two factors (eye movement and breath) will have created.
On exhalation and complete relaxation, the head/neck is taken to a new barrier and the process repeated. If the shoulder is brought into the equation, this is firmly held as it attempts to lightly push into a shrug. After this 10 second contraction the muscle will have released somewhat and slack can again be taken out as the head is repositioned before a repetition of the procedure commences.
Dr. Alex Jimenez offers an additional assessment and treatment of the hip flexors as a part of a referenced clinical application of neuromuscular techniques by Leon Chaitow and Judith Walker DeLany. The scope of our information is limited to chiropractic and spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
By Dr. Alex Jimenez

Additional Topics: Wellness
Overall health and wellness are essential towards maintaining the proper mental and physical balance in the body. From eating a balanced nutrition as well as exercising and participating in physical activities, to sleeping a healthy amount of time on a regular basis, following the best health and wellness tips can ultimately help maintain overall well-being. Eating plenty of fruits and vegetables can go a long way towards helping people become healthy.

WELLNESS TOPIC: EXTRA EXTRA: Managing Workplace Stress
References
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Assessment and Treatment of Upper Trapezius" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



