These assessment and treatment recommendations represent a synthesis of information derived from personal clinical experience and from the numerous sources which are cited, or are based on the work of researchers, clinicians and therapists who are named (Basmajian 1974, Cailliet 1962, Dvorak & Dvorak 1984, Fryette 1954, Greenman 1989, 1996, Janda 1983, Lewit 1992, 1999, Mennell 1964, Rolf 1977, Williams 1965).
Clinical Application of Neuromuscular Techniques: Levator Scapulae (As Seen on Fig. 4.36 Below)
Assessment of the Levator Scapulae
Levator scapula ‘springing’ test (a) The patient lies supine with the arm of the side to be tested stretched out with the supinated hand and lower arm tucked under the buttocks, to help restrain movement of the shoulder/scapula. The practitioner’s contralateral arm is passed across and under the neck to cup the shoulder of the side to be tested, with the forearm supporting the neck. 11 The practitioner’s other hand supports the head. The forearm is used to lift the neck into full pain-free flexion (aided by the other hand). The head is placed fully towards side-flexion and rotation, away from the side being treated.
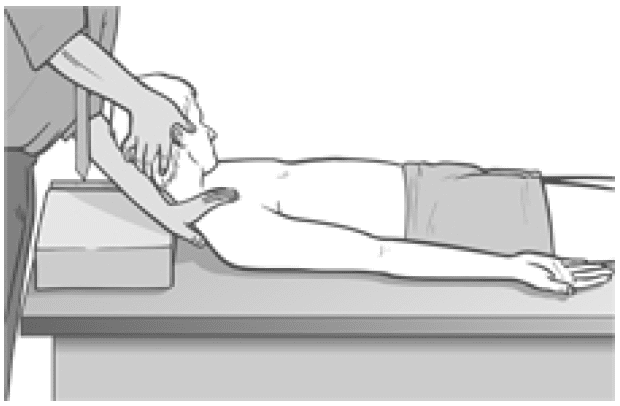
Figure 4.36 MET test (a) and treatment position for levator scapula (right side).
With the shoulder held caudally and the head/ neck in the position described (each at its resistance barrier) stretch is being placed on levator from both ends.
If dysfunction exists and/or levator scapula is short, there will be discomfort reported at the attachment on the upper medial border of the scapula and/or pain reported near the levator attachment on the spinous process of C2.
The hand on the shoulder gently ‘springs’ it caudally.
If levator is short there will be a harsh, wooden feel to this action. If it is normal there will be a soft feel to the springing pressure.
Levator scapula observation test (b) A functional assessment involves applying the evidence we have seen (see Ch. 2) of the imbalances which commonly occur between the upper and lower stabilisers of the scapula. In this process shortness is noted in pectoralis minor, levator scapulae and upper trapezius (as well as SCM), while weakness develops in serratus anterior, rhomboids, middle and lower trapezius – as well as the deep neck flexors.
Observation of the patient from behind will often show a ‘hollow’ area between the shoulder blades, where interscapular weakness has occurred, as well as an increased (over normal) distance between the medial borders of the scapulae and the thoracic spine, as the scapulae will have ‘winged’ away from it.
Levator scapula test (c) To see the imbalance described in test (b) in action, Janda (1996) has the patient in the press-up position (see Fig. 5.15). On very slow lowering of the chest towards the floor from a maximum push-up position, the scapula(e) on the side(s) where stabilisation has been compromised will move outwards, laterally and upwards – often into a winged position – rather than towards the spine.
This is diagnostic of weak lower stabilisers, which implicates tight upper stabilisers, including levator scapulae, as inhibiting them.
MET Treatment of Levator Scapula (Fig. 4.36)
Treatment of levator scapulae using MET enhances the lengthening of the extensor muscles attaching to the occiput and upper cervical spine. The position described below is used for treatment, either at the limit of easily reached range of motion, or a little short of this, depending upon the degree of acuteness or chronicity of the dysfunction.
The patient lies supine with the arm of the side to be tested stretched out alongside the trunk with the hand supinated. The practitioner, standing at the head of the table, passes his contralateral arm under the neck to rest on the patient’s shoulder on the side to be treated, so that the practitioner’s forearm supports the patient’s neck. The practitioner’s other hand supports and directs the head into subsequent movement (below).
The practitioner’s forearm lifts the neck into full flexion (aided by the other hand). The head is turned fully into side-flexion and rotation away from the side being treated.
With the shoulder held caudally by the practitioner’s hand, and the head/neck in full flexion, sideflexion and rotation (each at its resistance barrier), stretch is being placed on levator from both ends.
The patient is asked to take the head backwards towards the table, and slightly to the side from which it was turned, against the practitioner’s unmoving resistance, while at the same time a slight (20% of available strength) shoulder shrug is also asked for and resisted.
Following the 7–10 second isometric contraction and complete relaxation of all elements of this combined contraction, the neck is taken to further flexion, sidebending and rotation, where it is maintained as the shoulder is depressed caudally with the patient’s assistance (‘as you breathe out, slide your hand towards your feet’). The stretch is held for 20–30 seconds.
The process is repeated at least once.
CAUTION: Avoid overstretching this sensitive area.
Facilitation of Tone in Lower Shoulder Fixators Using Pulsed MET (Ruddy 1962)
In order to commence rehabilitation and proprioceptive re-education of a weak serratus anterior:
The practitioner places a single digit contact very lightly against the lower medial scapula border, on the side of the treated upper trapezius of the seated or standing patient. The patient is asked to attempt to ease the scapula, at the point of digital contact, towards the spine (‘press against my finger with your shoulder blade, towards your spine, just as hard [i.e. very lightly] as I am pressing against your shoulder blade, for less than a second’).
Once the patient has learned to establish control over the particular muscular action required to achieve this subtle movement (which can take a significant number of attempts), and can do so for 1 second at a time, repetitively, they are ready to begin the sequence based on Ruddy’s methodology (see Ch. 10, p. 75).
The patient is told something such as ‘now that you know how to activate the muscles which push your shoulder blade lightly against my finger, I want you to try do this 20 times in 10 seconds, starting and stopping, so that no actual movement takes place, just a contraction and a stopping, repetitively’.
This repetitive contraction will activate the rhomboids, middle and lower trapezii and serratus anterior – all of which are probably inhibited if upper trapezius is hypertonic. The repetitive contractions also produce an automatic reciprocal inhibition of upper trapezius, and levator scapula.
The patient can be taught to place a light finger or thumb contact against their own medial scapula (opposite arm behind back) so that home application of this method can be performed several times daily.
Treatment for Eye Muscles (Ruddy 1962)
Ruddy’s treatment method for the muscles of the eye is outlined in the notes below.
Ruddy’s Treatment for the Muscles of the Eye (Ruddy 1962)
Osteopathic eye specialist Dr T. Ruddy described a practical treatment method for application of MET principles to the muscles of the eye:
- The pads of the practitioner’s index, middle and ring finger and the thumb are placed together to form four contacts into which the eyeball (eye closed) can rest (middle finger is above the cornea and the thumb pad below it).
- These contacts resist the attempts the patient is asked to make to move the eyes downwards, laterally, medially and upwards – as well as obliquely between these compass points – up and half medial, down and half medial, up and half lateral, down and half lateral, etc.
- The fingers resist and obstruct the intended path of eye motion.
- Each movement should last for a count ‘one’ and then rest between efforts for a similar count, and in each position there should be 10 repetitions before moving on around the circuit. Ruddy maintained the method released muscle tension, permitted better circulation, and enhanced drainage. He applied the method as part of treatment of many eye problems.
Dr. Alex Jimenez offers an additional assessment and treatment of the hip flexors as a part of a referenced clinical application of neuromuscular techniques by Leon Chaitow and Judith Walker DeLany. The scope of our information is limited to chiropractic and spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
By Dr. Alex Jimenez

Additional Topics: Wellness
Overall health and wellness are essential towards maintaining the proper mental and physical balance in the body. From eating a balanced nutrition as well as exercising and participating in physical activities, to sleeping a healthy amount of time on a regular basis, following the best health and wellness tips can ultimately help maintain overall well-being. Eating plenty of fruits and vegetables can go a long way towards helping people become healthy.

IMPORTANT TOPIC: EXTRA EXTRA: A Healthier You!
OTHER IMPORTANT TOPICS: EXTRA: Sports Injuries? | Vincent Garcia | Patient | El Paso, TX Chiropractor
Post Disclaimer *
Professional Scope of Practice *
The information herein on "Assessment and Treatment of the Levator Scapulae" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Fitness, Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multistate Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Verify Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
RN: Registered Nurse
APRNP: Advanced Practice Registered Nurse
FNP: Family Practice Specialization
DC: Doctor of Chiropractic
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics



